If you are a caregiver of someone with Alzheimer’s disease (AD), you know it can sometimes be difficult for both of you to get adequate sleep. This lack of sleep is associated with memory loss and trouble thinking (1), which is detrimental to both you and the person living with AD (PLWD).
In this article, we’ll look at how AD impacts sleep and some of the sleep issues people with AD experience. In addition, we’ll provide expert tips on how you can help improve the sleep quality of persons living with AD. We’ll also discuss ways you, as the caregiver, can get better sleep.
Note: These general recommendations should not be taken as medical advice. If you have any health-related questions regarding sleep, consult your physician or a trained medical professional.
The Relationship Between Alzheimer’s Disease and Sleep
Chronic lack of sleep over time has been linked to an increased risk for developing Alzheimer’s disease. (2) In a study of men between the ages of 50 and 70, those who experienced sleep disturbances were 51% more likely to develop AD as opposed to those who had quality, restful sleep. (3) For individuals who have developed AD, sleep issues are common.
“Disturbed sleep can also be a prodrome, or an early symptom indicating the onset of a neurological disease such as AD,” says Christina Pierpaoli Parker, PhD, a postdoctoral fellow of Behavioral Medicine and Clinical Psychology at the University of Alabama at Birmingham.
Research suggests that sleep disturbances may also have a significant impact in advancing the progression of AD. (4) As AD progresses, sleep issues such as obstructive sleep apnea (5) can worsen. (6)
“Growing evidence suggests that sleep may play a critical role in the clearance of neurotoxins, including beta-amyloid, implicated in Alzheimer’s disease and related dementias,” adds Pierpaoli Parker. (7)
Sleeping with Alzheimer’s Disease
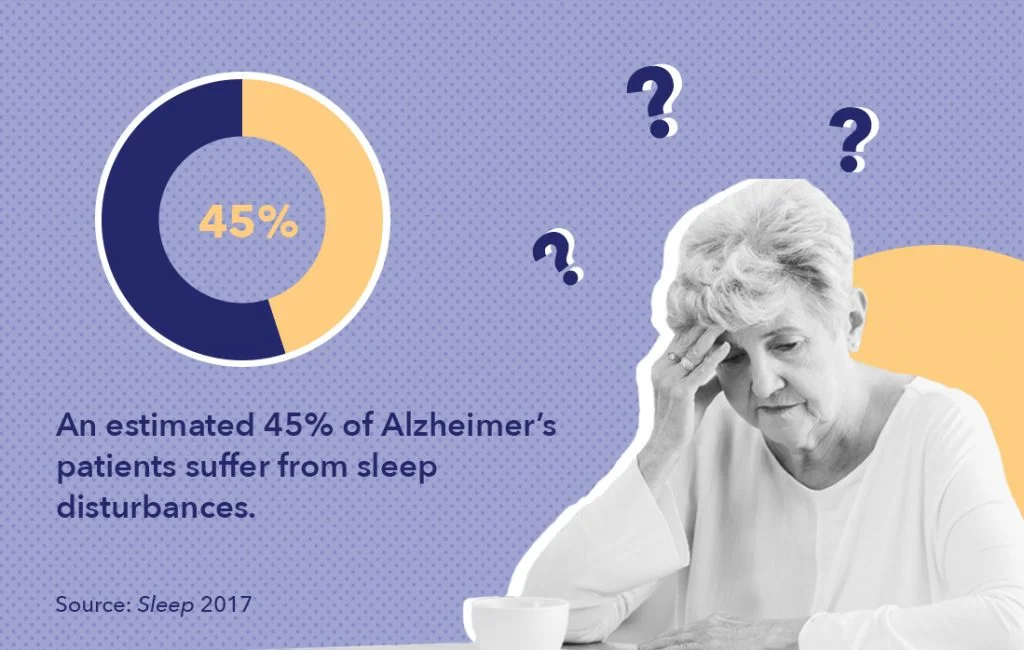
According to a 2017 study in Sleep, an estimated 45% of people with Alzheimer’s suffer from sleep disturbances. (8) When compared to other older adults, people with Alzheimer’s disease are much more likely to experience sleep issues. (9) Teresa Crawford, owner and operator of The Creeks memory support residences, says if they can’t sleep, the person with AD may have trouble lying still, become irritated, or wander at night.
These common behaviors may keep caregivers on edge and hypervigilant in the evening especially, contributing to their own difficulties initiating and maintaining sleep, notes Pierpaoli Parker.
Individuals with Alzheimer’s may experience feeling aroused at night, have difficulty falling asleep, consistently wake up in the middle of the night, and/or wake up too early. As a result, they may feel tired the next day and have the desire to take frequent naps. (10)
Sundowning
According to Sarah Johnson, geriatric RN and the health ambassador for Family Assets, one of the most common ways that Alzheimer’s interrupts sleep is through what is often referred to as the “sundowning” phenomenon. Sundowning occurs when people with AD start to feel restless, anxious, confused, and irritated at dusk. She says these feelings last the entire night, causing sleep difficulties.
One way to combat sundowning is by regular physical exercise, which can improve a person’s mood. (11)
“Some research also suggests that supplementing with a low dose of melatonin, alone or in combination with bright light therapy during the day, may help manage sundowning symptoms and related agitation (12),” adds Chrisitna Pierpaoli Parker.
Senior Isolation
Seniors who experience isolation and loneliness are more likely to have sleep issues and avoid exercise (13), and social isolation may worsen both. Online social support platforms designed to reduce isolation among seniors show promise for reducing perceived loneliness (14) and suggest that increased social activity— whether online or in-person — plays a critical role in combating isolation among this population.
While routines have significant psychiatric and physical health benefits for older adults with (and without) sleep concerns, those devoid of social activity may increase perceived loneliness in this population (15) and maintain sleep disturbances.
Ways to Improve Sleep for People With Alzheimer’s
Even though sleep can be difficult for people with AD, there are ways to mitigate these issues. Here are a few ways you can help someone with AD sleep easier:
- Establish morning and evening routines
- Create the right environment
- Exercise
- Perform calming activities
- Interact with others and learn about sleep hygiene
- Consider what they eat/drink before bedtime
- Avoid using medications if possible
Establish Morning and Evening Routines
Nurse Johnson notes that caregivers can create and maintain consistent morning and evening routines, which are especially helpful to those suffering cognitive decline. This can include keeping a regular wake time and tending to the person’s hygiene needs first thing in the morning when they are more alert. Additionally, an evening routine might involve reducing sensory stimulation as the night progresses and creating a relaxing bedtime ritual.
Create the Right Environment
Rachel Ann, an occupational therapist at Fitness About, says to provide a familiar bedroom by displaying photos or other mementos that the PLWD may recognize. She also says to avoid moving the furniture around so that their bedroom stays familiar.
Keeping a small night light on to reduce agitation associated with dark, unfamiliar settings (i.e. in assisted living facilities, nursing homes) may also help.
Having a comfortable mattress is necessary for the optimal sleeping conditions. Since each person’s sleep preferences are going to depend on factors such as their age, weight, and preferred sleep position, it’s important that you find the right mattress for them.
Annette Fields, executive director of the Vineyard Johns Creek assisted living community says creating a safe environment is also incredibly important. She recommends the following:
- Have working smoke alarms throughout the house
- Put a lamp that is easy to turn on within reach of the bed
- Remove trip hazards such as area rugs
- Lock all windows and doors to the outside before bedtime
- Place a non-spillable water bottle beside the bed in case the person in your care wakes up thirsty
Teresa Crawford suggests placing nightlights in the bedrooms, halls, and bathrooms. She says this will help the person feel safe when walking at night and help them to establish a healthy bedtime routine.
Exercise and Meditate
Persons with AD should exercise 3-5 times a week for 30 to 60 minutes at a time. (16) Caregivers can use familiar music or join in the exercise (such as by going on a walk) to make it more fun for the person with AD. If the individual has trouble walking, consider using exercise balls, stress bands, or light weights to help them get active. (17)
Growing research indicates that persons with dementia can also benefit from holistic programs that include adapted, gentle exercises such as yoga and tai chi. “Exercising in bright or natural light earlier in the day can help to regulate the body’s circadian rhythm, or biological clock,” says Pierpaoli Parker.
Teresa Crawford agrees. She says exercise or other tasks that require more energy should occur in the morning. This can promote sleepiness later in the day. She notes, however, that naps should be limited to maintain a healthy wake/sleep schedule, though the occasional brief (i.e., 15-20 minutes) and consistent nap is fine.
Perform Calming Activities
Steven Michael Barlam, a licensed clinical social worker and CEO of JFS Care, recommends you and the person with dementia practice mindfulness activities during the day. These can include calming activities such as breathing exercises, listening to soft music, heating up a warm towel, or using a bed warmer.

He says it’s important to remain calm. This is because your state of mind is perceived by the person with AD, and it can be contagious.
Interact With Others and Learn About Sleep Hygiene
According to an article in Current Treatment Options in Neurology, structured social interactions have been shown to help people with AD sleep better. Sleep issues can arise from feelings of stress or loneliness as a result of little-to-no social activity. In addition, educating yourself and/or the PWD about proper sleep hygiene can promote more restful sleep.
Consider What They Eat/Drink Before Bedtime
Clinical social worker Steven Michael Barlam recommends folks with AD avoid caffeinated beverages and avoid eating right before bedtime. He also suggests making sure the person with AD uses the bathroom before going to bed.
Avoid Using Medications if Possible
It’s best to avoid using sleep medications if possible. At the very least, caution should be exercised when administering hypnotic drugs and benzodiazepines, which have strong contraindications for PLWD and older adults’ caregivers, alongside the PLWD’s care team, should carefully weigh the risks and benefits of using such medications before dispensing them. (18)
Improving Sleep for Caregivers of Persons With Alzheimer’s
Nurse Johnson notes that 94% of AD caregivers are sleep deprived. Occupational Therapist Rachel Ann says this is because caregivers must constantly be attending to the person with AD to keep them safe.
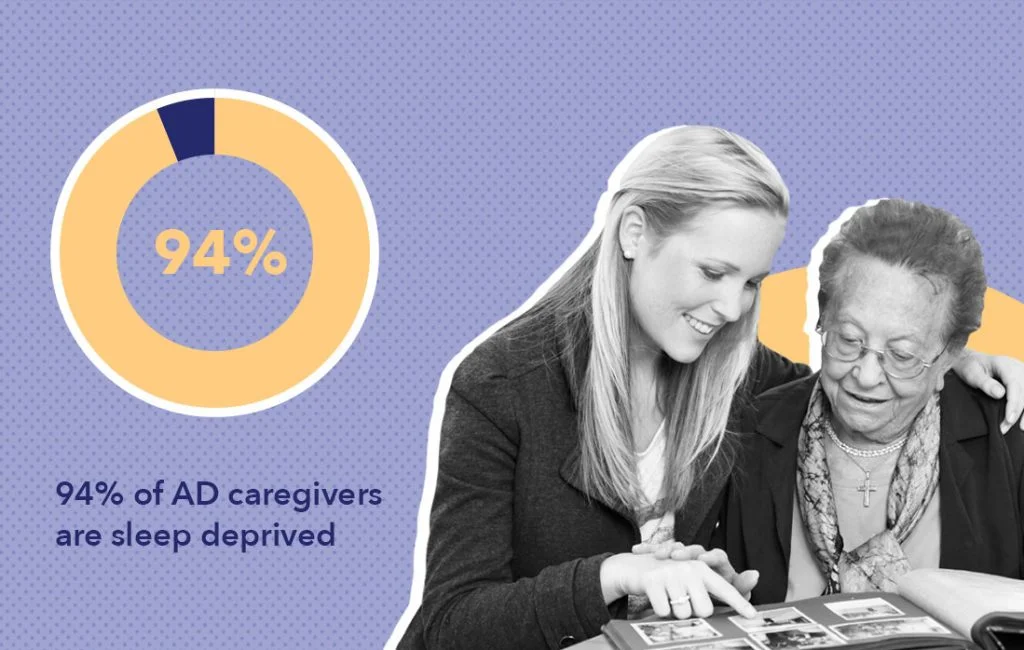
As someone who helped take care of her mother with AD for 20 years, Jennifer Fink, creator of the Fading Memories Podcast, is well aware of the sleep deprivation that occurs. Concerns about evening wandering common among PLWD can drive many caregivers’ sleep issues. Since people with AD may not be aware of the physical help they need, they might fall, scream, or have toileting issues at night, requiring you to help them instead of sleeping. This lack of sleep can be detrimental to the health of caregivers, since it can lead to making poor decisions or mistakes that could have been avoided with enough shut-eye.
Fink says she learned through experience one of the reasons people with AD struggle to understand the time of day: “One of the main warning signs of Alzheimer’s is difficulty with time and space. Eventually the disease affects the brain in a way that causes the person living with the disease to lose the concept of time and seasons. I was somewhat stunned by two very visual examples of seasons that my mom was oblivious to. The first was the change from spring to summer. Most of the year we have brown hills. It’s only during the winter and early spring that we have green hills. This change didn’t register with her even when she specifically stated how much she liked the hills. The other incident was Christmas. I took her to lunch in a place with a 20-foot Christmas tree and lots of decorations. She was completely surprised to be told it was December/Christmas time. Obviously, if someone is this unaware of the season it’s easy to understand that they have no concept of the time of day. ”
If you’re in a similar situation as Jennifer Fink, and you want to sleep better, consider the following:
- Use non-pharmacological approaches
- Talk to your doctor
- Take turns sharing caregiving responsibilities if possible
- Talk to a social worker or an Alzheimer’s Association representative
Use Non-Pharmacological Approaches
If you want to use non-pharmacological approaches to improve sleep, try to do the following:
- Exercise during the day
- Practice stress management exercises such as stretching and yoga
- Improve your sleep hygiene through education and practice (19), as well as seeking out Cognitive Behavioral Therapy for Insomnia (CBT-I), an evidence-based, short-term treatment for chronic insomnia–one of the most common sleep concerns among dementia caregivers.

Clinical social worker Steven Michael Barlam suggests:
- Making sure you get enough uninterrupted sleep prior to your shifts
- Taking naps when the person in your care is napping
- Meditating so you can build internal strength
Talk to Your Doctor
Jennifer Fink says she never had a doctor ask how she was doing while she was taking care of her mother. As such, it’s important to speak to a doctor, especially if you’re experiencing symptoms such as anxiety and depression as a result of a lack of sleep. Doing so will allow them to create a tailored approach to help improve your rest. (20)
Take Turns if Possible
Occupational Therapist Rachel Ann recommends caregivers take turns with someone, such as a family member, if possible. By having someone help share the load, you may be more likely to get quality rest.
As someone who helped care for his father with AD, Gary Joseph LeBlanc, Educational Director of the Dementia Spotlight Foundation, says caregivers are going to need help. He also says not to feel guilty asking for help, because “Heading into the later stage of Alzheimer’s, this no longer becomes a one-caregiver job. Even if you get someone to come by and sit with your loved one for 2-3 hours, take advantage of it and try to get some undisrupted sleep. You are going to need it, and you deserve it.”
Talk to a Social Worker or an Alzheimer’s Association Representative
If you aren’t able to get help from a family member, Teresa Crawford suggests speaking to a social worker or a representative of a local Alzheimer’s Association to see what support may be available to you.

If there is not an Alzheimer’s Association group in your area, they also provide the option of meeting virtually with a group.
Last Word From Sleepopolis
Having AD or caring for someone with this disease can have a negative impact on sleep. It’s important to take care of not just the person living with AD but yourself. Non-pharmacological approaches such as exercise and practicing good sleep hygiene can help both you and the person in your care. Also, there’s no need to feel guilty if you ask for help with caregiving duties. Taking a break to sleep can help you perform your caregiving duties better in the long run. Please keep in mind that we’re not medical professionals, so be sure to consult your healthcare provider with any medically related questions.
References
- “Reduce your risk for Alzheimer’s now.” Georgia Department of Public Health, https://dph.georgia.gov/reduce-your-risk-alzheimers-now
- “Not All Sleep is Equal When It Comes to Cleaning the Brain.” University of Rochester Medical Center, Feb 27, 2019. https://www.urmc.rochester.edu/news/story/not-all-sleep-is-equal-when-it-comes-to-cleaning-the-brain
- Benedict, C et al. Self-reported sleep disturbance is associated with Alzheimer’s disease risk in men. Alzheimer’s & Dementia. Sep 2015.
- Holth, J et al. Sleep in Alzheimer’s Disease–Beyond Amyloid. Neurobiology of Sleep and Circadian Rhythms. Jan 2017.
- Andrade, A et al. The relationship between Obstructive Sleep Apnea and Alzheimer’s Disease. Journal of Alzheimer’s Disease. 2018.
- Irwin, M et al. Implications of sleep disturbance and inflammation for Alzheimer’s disease dementia. The Lancet. Mar 2019.
- Shokri-Kojori, Ehsan, et al. “β-Amyloid Accumulation in the Human Brain after One Night of Sleep Deprivation.” Proceedings of the National Academy of Sciences, vol. 115, no. 17, 2018, pp. 4483–4488., doi:10.1073/pnas.1721694115.
- Bubu, O et al. Sleep, Cognitive impairment, and Alzheimer’s disease: A Systematic Review and Meta-Analysis. Sleep. Jan 1, 2017.
- Mander, B et al. Sleep: A novel mechanistic pathway, biomarker, and treatment target in the pathology of Alzheimer’s disease? Trends in Neurosciences. Aug 2016.
- Brzecka, A et al. Sleep Disorders Associated With Alzheimer’s Disease: A Perspective. Frontiers in Neuroscience. May 31, 2018.
- “Alzheimer’s Disease.” Us Department of Veterans Affairs, https://www.research.va.gov/topics/alzheimers.cfm
- Canevelli, M. Sundowning in Dementia: Clinical Relevance, Pathophysiological Determinants, and Therapeutic Approaches. Frontiers in Medicine. Dec 27, 2016.
- Shailey, M et al. Social isolation and loneliness in people aged 55 and over in Milton Keynes. The Open University. 2015.
- Arnaud, R et al. User-Centred Approach to Design an Online Social Support Platform for Seniors : Identification of Users’ Types and Their Requirements. Studies in Health Technology and Informatics. 2020.
- “2014 North County Senior Connections: Needs Assessment and Asset Mapping.” University of San Diego. https://digital.sandiego.edu/cgi/
- Ooms, S et al. Treatment of sleep disorders in dementia. Current Treatment Options in Neurology. Sep 1, 2017.
- “Staying Physically Active with Alzheimer’s.” National Institute on Aging. https://www.nia.nih.gov/health/staying-physically-active-alzheimers
- McCleery, J et al. Pharmacotherapies for sleep disturbances in dementia. Cochrane Database of Systematic Reviews. Nov 15, 2020.
- Gao, C et al. Sleep Duration and Sleep Quality in Caregivers of Patients With Dementia A Systematic Review and Meta-analysis. The Journal of the American Medical Association. Aug 23, 2019.
- Byun, E et al. How Adult Caregiving Impacts Sleep: a Systematic Review. Current Sleep Medicine Reports. 2016.

























