Long Story Short
- Sleep supports our metabolic health, and our internal clock plays a role in the organs that regulate glucose, lipid, and protein balance within our cells and our body. (1)
- Sleep deprivation and sleep disorders are associated with metabolic syndrome. (2)
- Sleep deprivation is all too common, with up to 40 percent of adults reporting insomnia symptoms. (2)
- Sleeping and eating outside of a typical circadian rhythm is associated with impaired glucose control and may increase the risk of diabetes, cardiovascular disease, and stroke long-term. (2)
- Some medications that treat symptoms of metabolic syndrome, like beta blockers, can negatively impact sleep, so it’s important to discuss sleep in conversations with a healthcare provider. (2)
- Some findings suggest that sleeping 7 to 7.5 hours per night is correlated with the lowest risk for metabolic syndrome and its negative outcomes. (2)
Metabolism is the process by which your body converts the things you eat and drink into energy to support everyday functions like breathing, digestion, and cell repair. Poor sleep can disrupt this process, leading to metabolic issues like weight gain, insulin resistance, and an increased risk of chronic conditions such as type 2 diabetes.
So, how can you improve both your sleep and metabolism? These two aspects of our health are actually deeply connected, and supporting both may be more straightforward than you think.
Note: The content on Sleepopolis is meant to be informative in nature, but it shouldn’t be taken as medical advice, and it shouldn’t take the place of medical advice and supervision from a trained professional. If you feel you may be suffering from any sleep disorder or medical condition, please see your healthcare provider immediately.
What Is Metabolic Health?
Metabolic health refers to how well your body processes and uses energy from the food you consume. This includes how efficiently your body manages important things like regulating your blood sugar levels, cholesterol, and blood pressure.
The body’s metabolism involves hormones, organs, and enzymes that work together to digest, absorb, process, transport, and even get rid of essential nutrients. (3) The liver is the central organ involved, but the adrenal gland, thyroid, and parathyroid (which is behind the thyroid and helps regulate calcium and phosphorus levels) also play an important role in metabolism. (4)(5)
When you’re in “good” metabolic health, this means that these systems are working smoothly and keeping your body in balance. This is essential because when everything is working properly, it lowers your risk of developing chronic diseases such as heart disease and type 2 diabetes. (6) Having good metabolic health is important for your overall wellness, improving energy levels and brain function while supporting weight management.
There are several primary markers of metabolic health: (7)
- Blood sugar and insulin levels: This shows how well your body regulates sugar in the blood, making sure it’s not too high or too low for a prolonged period (for instance, how well it delivers insulin to move glucose out of your blood). (8)
- Cholesterol and triglycerides: Healthy levels of these fats mean your heart and blood vessels are less at risk for damage and disease, including blockages that can lead to a heart attack or stroke.
- Blood pressure: Normal levels prevent strain on your heart and arteries.
- Waist circumference: A larger waist can signal higher levels of visceral fat (a type of deep belly fat) linked to poor metabolic health. (9)
When someone is not in good metabolic health, a cluster of conditions that add up to metabolic syndrome can develop. This includes high blood pressure, high blood sugar, abnormal blood fats, and excess fat around the waist — all of which raise your risk of heart disease, stroke, and type 2 diabetes. (10)
Having metabolic syndrome means that your body is struggling with key aspects of metabolic health. When these biomarkers are out of whack, it can be a warning sign for serious health issues if the underlying causes are left unaddressed. (7)
Some people have what is known as a fast metabolism (often stereotyped as a tall, skinny teenage boy, for instance) and other people have a slow metabolism. Your “metabolic speed” is passed down genetically. (11)
According to Mindy Pelz, DC, a nutrition and functional health expert, “A fast metabolism is really about two things: one is how well your metabolic organs can burn the glucose that enters your body from eating a meal.” A body that burns glucose well doesn’t need to store extra glucose as fat.
She continues, “The second is that once you burn through the glucose quickly, your body will burn fat for energy.” This process is known as metabolic switching, and it allows people to switch from burning sugar to burning fat quickly. (12)
Several life factors can have an impact on your metabolism, like getting older, pregnancy, your diet pattern, medications, and stress. And although many people don’t realize it, sleep can have an impact on metabolism.
The Link Between Sleep and Metabolism
Metabolism and sleep are deeply interconnected. Sleep is essential for regulating many of the hormonal and metabolic processes that keep your body functioning properly. One of the key connections between them is hormonal regulation.
Adrian Hernandez, MS, RDN, certified gastrointestinal dietitian and owner of AEH Nutrition LLC, explained that good quality sleep helps your body use insulin more effectively. It also supports the healthy regulation of appetite hormones (ghrelin and leptin) and helps reduce the stress hormone cortisol. These improvements decrease your risk of diabetes, cardiovascular disease, and obesity/weight resistance. (13)(14)
Getting enough quality sleep (at least 7-9 hours for adults) also allows your body to efficiently manage energy, hunger, and blood sugar. (14)(15) However, when you’re struggling in the sleep department, this balance can become disrupted. Eventually, this disruption can lead to insulin resistance, a condition in which your body becomes less effective at using insulin. This can cause elevated blood sugar levels and increase the risk of developing type 2 diabetes over time. (16)
Sleep is critical for our rest, repair, and regeneration. Things like muscle repair, cell growth, and fat burning all occur in deep sleep, making it essential for metabolic health. Poor sleep or sleep disorders (like sleep apnea) prevent your body from fully entering this restorative phase, which can impair metabolism and slow processes like fat burning and muscle repair. (17)
Your sleep and metabolic function are primarily controlled by your circadian rhythm, your body’s internal clock, or sleep-wake cycle. It’s influenced by outside factors like light and food, which signal your body when to sleep and when to be wakeful and active. Circadian rhythm can be disrupted by irregular sleep patterns, resulting in metabolic impairments that contribute to increased appetite, higher blood sugar levels, and unintentional weight gain. (18)
Poor sleep patterns or lack of sleep can also significantly affect your metabolism. Studies show that when you’re not adequately rested, hunger hormones rise and fullness hormones decline. An imbalance in these appetite-regulating hormones can trigger cravings for high-calorie, carbohydrate-rich foods, contributing to overeating and weight gain. Plus, a slowed metabolism from lack of sleep also means your body is less efficient at using energy, increasing the risk of weight-related challenges. (19)(20)
Finally, chronic sleep deprivation has been associated with a higher risk of developing serious health conditions, such as obesity, heart disease, type 2 diabetes, and certain cancers. The way that a lack of sleep disrupts insulin sensitivity and repair processes can set you up for a cycle that contributes to metabolic disorders. (21)(22)
Some research has even found a correlation between sleep deprivation and changes in how your body metabolizes fats. In other words, poor sleep may contribute to abnormal blood fat levels, which can increase the risk of heart disease. (23)
Are you getting enough sleep? One of the best ways to meet sleep goals and give your metabolic function a pick-me-up is to follow a consistent sleep schedule. For example, going to bed and waking up around the same times every day (even on the weekends). If you’re not sure where you fall with your sleep habits, our sleep calculator will provide insight into your ideal sleep schedule based on the number of sleep cycles you’re likely to attain.
Does Your Metabolism Slow Down When You Sleep?
Yes, your metabolism slows down while you sleep, but it doesn’t turn off just because your consciousness does. When you’re sleeping, your body uses less energy, and fewer calories are needed for functions like breathing, circulation, and cell repair. (24)
Still, your body continues to use energy to support essential functions like maintaining optimal body temperature, repairing tissues, and supporting brain activity during sleep cycles.
Do You Lose Weight When You Sleep?
Technically, yes, you lose weight while you sleep, but the majority of it is water weight (not fat). As you breathe and sweat during sleep, your body loses fluids (called “insensible water loss”) which can result in a small reduction in weight by morning compared to, say, the day before. (25)(26)
In a broader sense, sleep is involved in long-term weight management goals because of how it supports healthy metabolic functions, like managing your appetite-regulating hormones. Getting enough sleep helps reduce hunger and cravings while improving insulin sensitivity. (27)
Poor sleep can have the opposite effect, making weight management more challenging. While the act of sleeping itself doesn’t burn significant amounts of fat, it’s an essential piece of maintaining a healthy weight and supporting overall metabolic health. (13)
Ways to Support Both Your Sleep and Metabolism
Now that we’ve covered the two-way relationship between your sleep quality and your metabolism, let’s get into the actionable stuff. What can you do to help make sure you’re getting the most out of both of these things?
Below, you’ll find our curated tips for optimizing your sleep and metabolic function at the same time. Just note that for the most benefit, these tips should be used alongside other measures that support your overall wellness, like eating a healthy diet, moving your body, and practicing good sleep hygiene habits.
Plan for Your Circadian Rhythm
Aligning your eating habits with your circadian rhythm can significantly improve both your metabolism and sleep quality. The circadian rhythm is your body’s internal clock, regulating cycles of sleep, energy, and digestion based on the 24-hour day. Eating in sync with this rhythm can optimize digestion and energy use while eating late or irregularly can disrupt these processes and contribute to metabolic issues like weight gain and metabolic syndrome. (28)
Eating earlier in the day, when your metabolism is naturally more active, helps your body digest food efficiently and convert it into energy. Consuming large meals late at night, on the other hand, can interfere with both digestion and sleep. Late-night eating forces your body to focus on digestion instead of repair and recovery, leading to disrupted sleep and slower metabolism. (29)
If possible, Hernandez recommends avoiding meals 2-3 hours before bed so that your body has adequate time to digest. He notes, “Tryptophan, melatonin, and serotonin are really important components to quality sleep.”
Tryptophan is an amino acid found in animal proteins like fish, eggs, dairy, meats, and poultry. Diets low in tryptophan have been associated with worsened sleep. (30) It also helps with the production of serotonin — AKA the “happy” brain chemical involved in hunger, memory, and sleep regulation. Hernandez explains that serotonin doesn’t come from food, but its production is enhanced through exercise and sunshine.
He continues, “Melatonin is the hormone that controls your sleep cycles and is what is released from the body when light/sunlight begins to decrease. When the lights come up, your melatonin production decreases, stimulating the wake response.” (31)
To support both sleep and metabolic function, aim to eat your largest meals during daylight hours, if that makes sense for your needs and lifestyle. If it works for you, stick to lighter, nutrient-rich snacks in the evening, like a banana with almond butter or a Greek yogurt with berries, to prevent overburdening your digestive system and promote restful sleep. This approach keeps your metabolism aligned with your circadian rhythm, supporting optimal energy use and better sleep quality. (32)(33)
Address Stress
Stress has a significant negative impact on metabolic health. Research shows that chronic stress elevates cortisol levels, which can lead to insulin resistance, increased fat storage, and a slowed metabolism, raising the risk of metabolic syndrome. Stress also triggers unhealthy eating habits, like overeating or choosing high-calorie comfort foods, further straining metabolic health. (34)
Stress can make you sleep worse and for less time. In addition to your mind racing, high cortisol levels make it difficult to relax, and chronic stress can lead to insomnia or frequent waking during the night. (35) Plus, chronic stress and poor sleep can encourage metabolic syndrome. (36)
Managing stress is complex and involves more than quick fixes like using essential oils or practicing yoga only when you’re already feeling overwhelmed. Addressing the root causes of stress requires intentional, sustainable changes to your lifestyle.
Some of Hernandez’s favorite stress management practices include mindful meditation (you might consider guided meditation apps), journaling, reading, and positive affirmations.
He says, “If you have the ability, set up ‘do not disturb’ to automatically turn on 2 hours before bed [on your phone]. You can also set screen time restrictions if you have that capability to help keep you accountable.” If that kind of limit feels like too much too fast, he recommends you start with a goal of adjusting by 15-20 minute increments.
Here are some other wellness practices that may help you manage stress effectively:
- Use habit-stacking: Integrate self-care activities, like deep breathing or stretching, into your existing routines (e.g., while brushing your teeth or making coffee). This way, you don’t have to carve out separate space for a new habit. (37)
- Start your day with mindfulness: Practice a quick morning meditation or set positive affirmations before work. The more consistently you do it, the more routine it will become. (38)
- Schedule breaks: Set boundaries by scheduling time for yourself throughout the day, away from work or responsibilities. Perhaps setting an audible alarm or visual calendar reminder can help. (39)
- Journal regularly: Use journaling to reflect on your stressors and identify patterns in your emotional health. You might even do a “brain dump” before bed to help clear your mind. (40)
- Prioritize meaningful social connections: Engage with supportive friends or loved ones to decompress and feel grounded. Social support is associated with better mental health and sleep outcomes, which can also support metabolic health. (41) (42)
Track Supplements and Medicines
Many people take a combination of supplements, over-the-counter medicines, and prescriptions for various health reasons. However, these things can interact and lead to unintended side effects that could impact both sleep and metabolic health.
Certain drugs prescribed for metabolic conditions, like stimulants or weight-loss medications, can negatively affect sleep. For example, some medications that support metabolism may trigger insomnia or poor sleep quality. Additionally, short sleep duration (less than 6 hours) among sleeping pill users is linked to metabolic syndrome. (43) (44)
To avoid these potential issues, it’s essential to track everything you’re taking and disclose them to your healthcare provider, especially before adding anything new.
Move Your Body
Physical activity boosts metabolism by increasing muscle mass and burning calories. Regular movement also improves insulin sensitivity, supports fat burning, and promotes overall metabolic health. It’s also protective against metabolic disease. (45)
Exercise also benefits your sleep quality. It helps keep your circadian rhythm on track by promoting energy during the day and relaxation at night. People who engage in regular physical activity often fall asleep faster, enjoy deeper sleep, and experience fewer disturbances throughout the night. (46)
For those with busy schedules, here are easy ways to incorporate movement into your day:
- Take movement breaks: It can be surprising to realize how much time we spend sitting down during the day (usually for work). Set a timer to stand up and walk for 5-10 minutes every hour, whether at work or home. It can be as simple as pacing around the office or house.
- Stretch or exercise while watching TV: Use downtime like watching TV or during phone calls to do light stretching or bodyweight exercises like squats or lunges. You could also use resistance bands or dumbbells.
- Walk and talk: Take walking meetings or phone calls to stay active while handling work or catching up with friends.
Support Your Gut
A healthy gut microbiome is essential for both sleep and metabolism. The gut is home to trillions of bacteria that help digestion and influence sleep behavior and metabolic function. (47)
Some research has found that an imbalanced gut microbiome (called dysbiosis) can disrupt sleep, which in turn influences metabolic processes. (13) Dysbiosis impairs the body’s ability to absorb nutrients and produce serotonin and melatonin effectively, making it harder to maintain healthy sleep and metabolism. (48)(49)
According to Hernandez, a well-balanced diet full of fruits, vegetables, lean proteins, and complex carbohydrates is essential to a happy gut and sleep. He says to focus first on fiber, which is important in the production of serotonin (95 percent of which is made in your gut) as well as reducing inflammation. “High-fiber foods also regulate blood sugar, which can prevent irregularities overnight that disrupt your sleep cycle.” (50) (51)
Hernandez also notes that some research shows sleep loss may be impacted by the overgrowth of certain bacteria in the gut. “Probiotic-rich foods like kefir, yogurt, kimchi, and pickled vegetables may be helpful in boosting your beneficial bacteria,” he says. (52)
To recap, support your gut health with these tips:
- Eat a fiber-rich diet: Include plenty of fruits, vegetables, whole grains, and legumes, which feed beneficial gut bacteria. (53)
- Consume fermented foods: Foods like yogurt, kimchi, sauerkraut, and kefir are rich in probiotics that help maintain a healthy gut microbiome. (54)
- Stay hydrated: Drinking enough water supports digestion and helps the gut function properly. (55)
- Limit ultra-processed foods: These types of foods, which tend to be high in added sugar and low in nutrients, may disrupt the balance of gut bacteria. (56)
- Consider a probiotic supplement: Talk to your healthcare provider about whether a probiotic could further support your gut health. (57)
For personalized nutrition recommendations, consider meeting with a registered dietitian who can help you come up with a plan.
Be Mindful of Blue Light
Blue light exposure in the evenings can negatively impact metabolic function, possibly by disrupting the hormones that regulate hunger and fullness. (58) Most of us get ample doses from our TVs, phones, handheld devices, and more.
Research shows that evening blue light exposure can lead to glucose peaks, impairing the body’s ability to regulate blood sugar, which could potentially increase the risk of metabolic syndrome. (59) (60)
Blue light can promote wakefulness during the day, but the downside is that it can also make it harder to fall asleep at night. Blue light also affects sleep by inhibiting the production of melatonin, the hormone that signals your body to prepare for rest. (61) While blue light-blocking filters and glasses are commonly used, there’s little evidence for their effectiveness. (62)(63)
Instead, here are some more effective ways to control blue light exposure:
- Limit screen time at night: Try to avoid using devices like smartphones, laptops, or tablets at least 1-2 hours before bedtime.
- Dim lights in the evening: Switch to warmer, dim lighting in your home after sunset to help your body prepare for sleep.
- Get natural sunlight during the day: Exposure to natural light during the daytime, especially first thing in the morning, helps regulate your circadian rhythm.
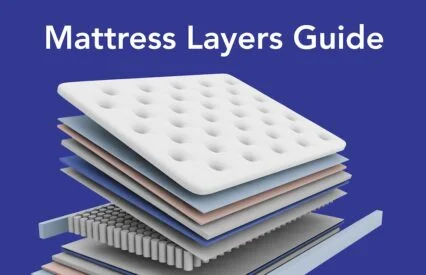
In addition to avoiding blue light, it helps to create a sleep-promoting environment in your bedroom. Consider factors like your mattress, pajamas, temperature, light, and overall comfort.
Use Caffeine Strategically
Many people rely on caffeine throughout the day to stay alert. Caffeine can also boost metabolism by increasing thermogenesis, the process of burning calories. However, it’s important to be intentional about your caffeine intake to avoid its potential negative effects.
“Caffeine is a stimulant that can provide your body with energy, but it can also cause headaches, insomnia, increased heart rate that leads to anxiety and fatigue in some individuals who are sensitive,” says Hernandez. (64) (65)
The Food and Drug Administration (FDA) recommends that healthy adults limit caffeine intake to a maximum of 400 milligrams (mg) per day. (66)
Hernandez offered the following examples of caffeine per serving of popular items: (67)
- 8oz of coffee: 80-100mg
- 8oz black tea: 30-50mg
- 12oz can of soda: 30mg
- 2 oz espresso shot: 120mg
Drinking caffeine on an empty stomach in the morning may impair your body’s ability to regulate blood sugar, leading to glucose spikes that may strain your metabolic health. Additionally, consuming caffeine too late in the day can make it hard to fall asleep and get quality rest, which is crucial for restoring metabolic function. (68)
Here are a few tips that can help you optimize your caffeine intake:
- Have caffeine with or after breakfast: This ensures that your body has food to help regulate blood sugar levels and prevent morning glucose spikes.
- Limit caffeine in the afternoon: Avoid drinking caffeinated beverages after noon to prevent disruptions to your sleep. Caffeine has a half-life of approximately five hours in adults, which means it can remain in your system for 10 hours after consuming it. (69)
- Opt for moderate consumption: Aim to keep your caffeine intake to less than 400 mg per day, which equates to about two to three 12-fluid-ounce cups of coffee. If you’re sensitive to caffeine, you should keep your coffee intake to just one or two cups per day and avoid drinking caffeine later in the day. (66)
FAQs
How does the amount of sleep you get affect your body and metabolism?
The amount of sleep you get directly impacts your body as well as appetite- and blood sugar-regulating hormones. Insufficient sleep can lead to increased appetite, weight gain, and a slower metabolism, raising the risk of obesity and related metabolic disorders.
Do you lose weight when you sleep?
Yes, technically you can lose weight while you sleep, but it’s primarily water weight lost through breathing and sweating {AKA “insensible weight loss”). Significant weight loss requires consistency from maintaining a healthy diet and active lifestyle, though regularly getting enough sleep is also an important factor.
Are sleep apnea and metabolism connected?
Sleep apnea disrupts sleep cycles, leading to hormonal imbalances that affect metabolism, including increased cortisol and insulin resistance. This can make weight loss more difficult and contribute to weight gain, raising the risk of metabolic disorders.
The Last Word from Sleepopolis
Several everyday things you can do to improve your metabolism can also help improve your sleep, and vice versa. If you’re looking to optimize your overall health, consider how you can boost the nutritional quality of your diet, keep extra stress at bay, move your body regularly, and practice good sleep hygiene — like following a regular sleep schedule, avoiding blue light at night, and keeping caffeine intake earlier in the day.
Making these types of lifestyle improvements can not only help you feel more rested but also support weight management goals and reduce your risk of metabolic syndrome.
Sources
- Sinturel, F., Petrenko, V., & Dibner, C. (2020). Circadian Clocks Make Metabolism Run. Journal of Molecular Biology, 432(12), 3680-3699. https://doi.org/10.1016/j.jmb.2020.01.018
- Chasens ER, Imes CC, Kariuki JK, Luyster FS, Morris JL, DiNardo MM, Godzik CM, Jeon B, Yang K. Sleep and Metabolic Syndrome. Nurs Clin North Am. 2021 Jun;56(2):203-217. doi: 10.1016/j.cnur.2020.10.012. Epub 2021 Mar 10. PMID: 34023116; PMCID: PMC8144542.
- Cleveland Clinic. (n.d.). Retrieved from: https://my.clevelandclinic.org/health/body/21893-metabolism
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. In brief: How does the liver work? [Updated 2023 Feb 28]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279393/
- Johns Hopkins Medicine. (n.d.). Anatomy of the Endocrine System. Retrieved from: https://www.hopkinsmedicine.org/health/wellness-and-prevention/anatomy-of-the-endocrine-system
- Oster H, Chaves I. Effects of Healthy Lifestyles on Chronic Diseases: Diet, Sleep and Exercise. Nutrients. 2023 Oct 31;15(21):4627. doi: 10.3390/nu15214627. PMID: 37960280; PMCID: PMC10650398.
- Swarup S, Ahmed I, Grigorova Y, et al. Metabolic Syndrome. [Updated 2024 Mar 7]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459248/
- Zhao, X., An, X., Yang, C., Sun, W., Ji, H., & Lian, F. (2023). The crucial role and mechanism of insulin resistance in metabolic disease. Frontiers in Endocrinology, 14, 1149239. https://doi.org/10.3389/fendo.2023.1149239
- Raheem, J., Sliz, E., Shin, J., Holmes, M. V., Pike, G. B., Richer, L., Gaudet, D., Paus, T., & Pausova, Z. (2022). Visceral adiposity is associated with metabolic profiles predictive of type 2 diabetes and myocardial infarction. Communications Medicine, 2(1), 1-7. https://doi.org/10.1038/s43856-022-00140-5
- Fahed G, Aoun L, Bou Zerdan M, Allam S, Bou Zerdan M, Bouferraa Y, Assi HI. Metabolic Syndrome: Updates on Pathophysiology and Management in 2021. Int J Mol Sci. 2022 Jan 12;23(2):786. doi: 10.3390/ijms23020786. PMID: 35054972; PMCID: PMC8775991.
- HarvardHealth Publishing. (2024). The Truth About Metabolism. Retrieved from: https://www.health.harvard.edu/staying-healthy/the-truth-about-metabolism
- Vasim I, Majeed CN, DeBoer MD. Intermittent Fasting and Metabolic Health. Nutrients. 2022 Jan 31;14(3):631. doi: 10.3390/nu14030631. PMID: 35276989; PMCID: PMC8839325.
- Papatriantafyllou E, Efthymiou D, Zoumbaneas E, Popescu CA, Vassilopoulou E. Sleep Deprivation: Effects on Weight Loss and Weight Loss Maintenance. Nutrients. 2022 Apr 8;14(8):1549. doi: 10.3390/nu14081549. PMID: 35458110; PMCID: PMC9031614.
- Liu S, Wang X, Zheng Q, Gao L, Sun Q. Sleep Deprivation and Central Appetite Regulation. Nutrients. 2022 Dec 7;14(24):5196. doi: 10.3390/nu14245196. PMID: 36558355; PMCID: PMC9783730.
- Chaput JP, Dutil C, Featherstone R, Ross R, Giangregorio L, Saunders TJ, Janssen I, Poitras VJ, Kho ME, Ross-White A, Carrier J. Sleep duration and health in adults: an overview of systematic reviews. Appl Physiol Nutr Metab. 2020 Oct;45(10 (Suppl. 2)):S218-S231. doi: 10.1139/apnm-2020-0034. PMID: 33054337.
- Singh T, Ahmed TH, Mohamed N, Elhaj MS, Mohammed Z, Paulsingh CN, Mohamed MB, Khan S. Does Insufficient Sleep Increase the Risk of Developing Insulin Resistance: A Systematic Review. Cureus. 2022 Mar 26;14(3):e23501. doi: 10.7759/cureus.23501. PMID: 35494895; PMCID: PMC9036496.
- Brinkman JE, Reddy V, Sharma S. Physiology of Sleep. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482512/
- Meyer N, Harvey AG, Lockley SW, Dijk DJ. Circadian rhythms and disorders of the timing of sleep. Lancet. 2022 Sep 24;400(10357):1061-1078. doi: 10.1016/S0140-6736(22)00877-7. Epub 2022 Sep 14. Erratum in: Lancet. 2023 May 13;401(10388):1570. doi: 10.1016/S0140-6736(23)00908-X. PMID: 36115370.
- Zhu B, Shi C, Park CG, Zhao X, Reutrakul S. Effects of sleep restriction on metabolism-related parameters in healthy adults: A comprehensive review and meta-analysis of randomized controlled trials. Sleep Med Rev. 2019 Jun;45:18-30. doi: 10.1016/j.smrv.2019.02.002. Epub 2019 Feb 10. PMID: 30870662.
- Gomes S, Ramalhete C, Ferreira I, Bicho M, Valente A. Sleep Patterns, Eating Behavior and the Risk of Noncommunicable Diseases. Nutrients. 2023 May 25;15(11):2462. doi: 10.3390/nu15112462. PMID: 37299426; PMCID: PMC10255419.
- Ramos AR, Wheaton AG, Johnson DA. Sleep Deprivation, Sleep Disorders, and Chronic Disease. Prev Chronic Dis. 2023 Aug 31;20:E77. doi: 10.5888/pcd20.230197. PMID: 37651644; PMCID: PMC10487788.
- Che T, Yan C, Tian D, Zhang X, Liu X, Wu Z. The Association Between Sleep and Metabolic Syndrome: A Systematic Review and Meta-Analysis. Front Endocrinol (Lausanne). 2021 Nov 19;12:773646. doi: 10.3389/fendo.2021.773646. PMID: 34867820; PMCID: PMC8640251.
- Gangitano E, Martinez-Sanchez N, Bellini MI, Urciuoli I, Monterisi S, Mariani S, Ray D, Gnessi L. Weight Loss and Sleep, Current Evidence in Animal Models and Humans. Nutrients. 2023 Aug 3;15(15):3431. doi: 10.3390/nu15153431. PMID: 37571368; PMCID: PMC10420950.
- Zhang, S., Tanaka, Y., Ishihara, A., Uchizawa, A., Park, I., Iwayama, K., Ogata, H., Yajima, K., Omi, N., Satoh, M., Yanagisawa, M., Sagayama, H., & Tokuyama, K. (2021). Metabolic flexibility during sleep. Scientific Reports, 11(1), 1-13. https://doi.org/10.1038/s41598-021-97301-8
- Weissenberg, S. (2005). INSENSIBLE WATER LOSS DURING SLEEP: A THEORETICAL EXERCISE. Advances in Physiology Education. https://doi.org/D0028-05
- Popkin BM, D’Anci KE, Rosenberg IH. Water, hydration, and health. Nutr Rev. 2010 Aug;68(8):439-58. doi: 10.1111/j.1753-4887.2010.00304.x. PMID: 20646222; PMCID: PMC2908954.
- Kline CE, Chasens ER, Bizhanova Z, Sereika SM, Buysse DJ, Imes CC, Kariuki JK, Mendez DD, Cajita MI, Rathbun SL, Burke LE. The association between sleep health and weight change during a 12-month behavioral weight loss intervention. Int J Obes (Lond). 2021 Mar;45(3):639-649. doi: 10.1038/s41366-020-00728-8. Epub 2021 Jan 7. PMID: 33414489; PMCID: PMC7914147.
- Chamorro R, Jouffe C, Oster H, Uhlenhaut NH, Meyhöfer SM. When should I eat: A circadian view on food intake and metabolic regulation. Acta Physiol (Oxf). 2023 Mar;237(3):e13936. doi: 10.1111/apha.13936. Epub 2023 Jan 27. PMID: 36645134.
- Han H, Dou J, Hou Q, Wang H. Role of Circadian Rhythm and Impact of Circadian Rhythm Disturbance on the Metabolism and Disease. J Cardiovasc Pharmacol. 2022 Mar 1;79(3):254-263. doi: 10.1097/FJC.0000000000001178. PMID: 34840256.
- Binks H, E Vincent G, Gupta C, Irwin C, Khalesi S. Effects of Diet on Sleep: A Narrative Review. Nutrients. 2020 Mar 27;12(4):936. doi: 10.3390/nu12040936. PMID: 32230944; PMCID: PMC7230229.
- Moon, E., Partonen, T., Beaulieu, S., & Linnaranta, O. (2022). Melatonergic agents influence the sleep-wake and circadian rhythms in healthy and psychiatric participants: A systematic review and meta-analysis of randomized controlled trials. Neuropsychopharmacology, 47(8), 1523-1536. https://doi.org/10.1038/s41386-022-01278-5
- Lopez-Minguez J, Gómez-Abellán P, Garaulet M. Timing of Breakfast, Lunch, and Dinner. Effects on Obesity and Metabolic Risk. Nutrients. 2019 Nov 1;11(11):2624. doi: 10.3390/nu11112624. PMID: 31684003; PMCID: PMC6893547.
- Hermenegildo-López Y, Donat-Vargas C, Sandoval-Insausti H, Moreno-Franco B, Rodríguez-Ayala M, Rey-García J, Banegas JR, Rodríguez-Artalejo F, Guallar-Castillón P. A Higher Intake of Energy at Dinner Is Associated with Incident Metabolic Syndrome: A Prospective Cohort Study in Older Adults. Nutrients. 2021 Aug 30;13(9):3035. doi: 10.3390/nu13093035. PMID: 34578912; PMCID: PMC8465293.
- Kivimäki M, Bartolomucci A, Kawachi I. The multiple roles of life stress in metabolic disorders. Nat Rev Endocrinol. 2023 Jan;19(1):10-27. doi: 10.1038/s41574-022-00746-8. Epub 2022 Oct 12. PMID: 36224493; PMCID: PMC10817208.
- Kuo WC, Ersig AL, Kunkul F, Brown RL, Oakley LD. Linking chronic stress to insomnia symptoms in older adults: The role of stress co-occurrence during the pandemic. Res Nurs Health. 2023 Feb;46(1):68-79. doi: 10.1002/nur.22278. Epub 2022 Nov 29. PMID: 36445114; PMCID: PMC9839487.
- Chaput JP, McHill AW, Cox RC, Broussard JL, Dutil C, da Costa BGG, Sampasa-Kanyinga H, Wright KP Jr. The role of insufficient sleep and circadian misalignment in obesity. Nat Rev Endocrinol. 2023 Feb;19(2):82-97. doi: 10.1038/s41574-022-00747-7. Epub 2022 Oct 24. PMID: 36280789; PMCID: PMC9590398.
- Cleveland Clinic. (2024). Everything You Need To Know About Habit Stacking for Self-Improvement. Retrieved from: https://health.clevelandclinic.org/habit-stacking
- Albalooshi S, Moeini-Jazani M, Fennis BM, Warlop L. Reinstating the Resourceful Self: When and How Self-Affirmations Improve Executive Performance of the Powerless. Pers Soc Psychol Bull. 2020 Feb;46(2):189-203. doi: 10.1177/0146167219853840. Epub 2019 Jun 11. PMID: 31185806; PMCID: PMC6931103.
- Albulescu P, Macsinga I, Rusu A, Sulea C, Bodnaru A, Tulbure BT. “Give me a break!” A systematic review and meta-analysis on the efficacy of micro-breaks for increasing well-being and performance. PLoS One. 2022 Aug 31;17(8):e0272460. doi: 10.1371/journal.pone.0272460. PMID: 36044424; PMCID: PMC9432722.
- Sohal M, Singh P, Dhillon BS, Gill HS. Efficacy of journaling in the management of mental illness: a systematic review and meta-analysis. Fam Med Community Health. 2022 Mar;10(1):e001154. doi: 10.1136/fmch-2021-001154. PMID: 35304431; PMCID: PMC8935176.
- Holt-Lunstad J. Social connection as a critical factor for mental and physical health: evidence, trends, challenges, and future implications. World Psychiatry. 2024 Oct;23(3):312-332. doi: 10.1002/wps.21224. PMID: 39279411; PMCID: PMC11403199.
- Kent de Grey RG, Uchino BN, Trettevik R, Cronan S, Hogan JN. Social support and sleep: A meta-analysis. Health Psychol. 2018 Aug;37(8):787-798. doi: 10.1037/hea0000628. Epub 2018 May 28. PMID: 29809022.
- Chasens ER, Imes CC, Kariuki JK, Luyster FS, Morris JL, DiNardo MM, Godzik CM, Jeon B, Yang K. Sleep and Metabolic Syndrome. Nurs Clin North Am. 2021 Jun;56(2):203-217. doi: 10.1016/j.cnur.2020.10.012. Epub 2021 Mar 10. PMID: 34023116; PMCID: PMC8144542.
- Izumida T, Nakamura Y, Sato Y, Ishikawa S. The Association Between Sleeping Pill Use and Metabolic Syndrome in an Apparently Healthy Population in Japan: JMS-II Cohort Study. J Epidemiol. 2022 Mar 5;32(3):145-150. doi: 10.2188/jea.JE20200361. Epub 2021 Mar 17. PMID: 33162423; PMCID: PMC8824657.
- Thyfault JP, Bergouignan A. Exercise and metabolic health: beyond skeletal muscle. Diabetologia. 2020 Aug;63(8):1464-1474. doi: 10.1007/s00125-020-05177-6. Epub 2020 Jun 11. PMID: 32529412; PMCID: PMC7377236.
- Kline CE, Hillman CH, Bloodgood Sheppard B, Tennant B, Conroy DE, Macko RF, Marquez DX, Petruzzello SJ, Powell KE, Erickson KI. Physical activity and sleep: An updated umbrella review of the 2018 Physical Activity Guidelines Advisory Committee report. Sleep Med Rev. 2021 Aug;58:101489. doi: 10.1016/j.smrv.2021.101489. Epub 2021 Apr 9. PMID: 33934046; PMCID: PMC8338757.
- Michels N, Zouiouich S, Vanderbauwhede B, Vanacker J, Indave Ruiz BI, Huybrechts I. Human microbiome and metabolic health: An overview of systematic reviews. Obes Rev. 2022 Apr;23(4):e13409. doi: 10.1111/obr.13409. Epub 2022 Jan 3. PMID: 34978141.
- Vaccaro R, Casini A, Severi C, Lamazza A, Pronio A, Palma R. Serotonin and Melatonin in Human Lower Gastrointestinal Tract. Diagnostics (Basel). 2023 Jan 5;13(2):204. doi: 10.3390/diagnostics13020204. PMID: 36673013; PMCID: PMC9857959.
- Sun J, Fang D, Wang Z, Liu Y. Sleep Deprivation and Gut Microbiota Dysbiosis: Current Understandings and Implications. Int J Mol Sci. 2023 May 31;24(11):9603. doi: 10.3390/ijms24119603. PMID: 37298553; PMCID: PMC10253795.
- Banskota S, Ghia JE, Khan WI. Serotonin in the gut: Blessing or a curse. Biochimie. 2019 Jun;161:56-64. doi: 10.1016/j.biochi.2018.06.008. Epub 2018 Jun 14. PMID: 29909048.
- Tang M, Song X, Zhong W, Xie Y, Liu Y, Zhang X. Dietary fiber ameliorates sleep disturbance connected to the gut-brain axis. Food Funct. 2022 Nov 28;13(23):12011-12020. doi: 10.1039/d2fo01178f. PMID: 36373848.
- Matenchuk BA, Mandhane PJ, Kozyrskyj AL. Sleep, circadian rhythm, and gut microbiota. Sleep Med Rev. 2020 Oct;53:101340. doi: 10.1016/j.smrv.2020.101340. Epub 2020 May 13. PMID: 32668369.
- Fu J, Zheng Y, Gao Y, Xu W. Dietary Fiber Intake and Gut Microbiota in Human Health. Microorganisms. 2022 Dec 18;10(12):2507. doi: 10.3390/microorganisms10122507. PMID: 36557760; PMCID: PMC9787832.
- Leeuwendaal NK, Stanton C, O’Toole PW, Beresford TP. Fermented Foods, Health and the Gut Microbiome. Nutrients. 2022 Apr 6;14(7):1527. doi: 10.3390/nu14071527. PMID: 35406140; PMCID: PMC9003261.
- Liska D, Mah E, Brisbois T, Barrios PL, Baker LB, Spriet LL. Narrative Review of Hydration and Selected Health Outcomes in the General Population. Nutrients. 2019 Jan 1;11(1):70. doi: 10.3390/nu11010070. PMID: 30609670; PMCID: PMC6356561.
- Whelan K, Bancil AS, Lindsay JO, Chassaing B. Ultra-processed foods and food additives in gut health and disease. Nat Rev Gastroenterol Hepatol. 2024 Jun;21(6):406-427. doi: 10.1038/s41575-024-00893-5. Epub 2024 Feb 22. PMID: 38388570.
- Gul S, Durante-Mangoni E. Unraveling the Puzzle: Health Benefits of Probiotics-A Comprehensive Review. J Clin Med. 2024 Mar 1;13(5):1436. doi: 10.3390/jcm13051436. PMID: 38592298; PMCID: PMC10935031.
- Driller MW, Jacobson G, Uiga L. Hunger hormone and sleep responses to the built-in blue-light filter on an electronic device: a pilot study. Sleep Sci. 2019 Jul-Sep;12(3):171-177. doi: 10.5935/1984-0063.20190074. PMID: 31890092; PMCID: PMC6932843.
- Ishihara A, Courville AB, Chen KY. The Complex Effects of Light on Metabolism in Humans. Nutrients. 2023 Mar 14;15(6):1391. doi: 10.3390/nu15061391. PMID: 36986120; PMCID: PMC10056135.
- Wahl S, Engelhardt M, Schaupp P, Lappe C, Ivanov IV. The inner clock-Blue light sets the human rhythm. J Biophotonics. 2019 Dec;12(12):e201900102. doi: 10.1002/jbio.201900102. Epub 2019 Sep 2. PMID: 31433569; PMCID: PMC7065627.
- Silvani MI, Werder R, Perret C. The influence of blue light on sleep, performance and wellbeing in young adults: A systematic review. Front Physiol. 2022 Aug 16;13:943108. doi: 10.3389/fphys.2022.943108. PMID: 36051910; PMCID: PMC9424753.
- Mayo Clinic Health System. (2022). Are blue light-blocking glasses a must-have? Retrieved from: https://www.mayoclinichealthsystem.org/hometown-health/speaking-of-health/are-blue-light-blocking-glasses-a-must-have
- Singh S, Keller PR, Busija L, McMillan P, Makrai E, Lawrenson JG, Hull CC, Downie LE. Blue-light filtering spectacle lenses for visual performance, sleep, and macular health in adults. Cochrane Database Syst Rev. 2023 Aug 18;8(8):CD013244. doi: 10.1002/14651858.CD013244.pub2. PMID: 37593770; PMCID: PMC10436683.
- Rodak K, Kokot I, Kratz EM. Caffeine as a Factor Influencing the Functioning of the Human Body-Friend or Foe? Nutrients. 2021 Sep 2;13(9):3088. doi: 10.3390/nu13093088. PMID: 34578966; PMCID: PMC8467199.
- Liu C, Wang L, Zhang C, Hu Z, Tang J, Xue J, Lu W. Caffeine intake and anxiety: a meta-analysis. Front Psychol. 2024 Feb 1;15:1270246. doi: 10.3389/fpsyg.2024.1270246. PMID: 38362247; PMCID: PMC10867825.
- US Food and Drug Administration. (2024). Spilling the Beans: How Much Caffeine is Too Much? Retrieved from: https://www.fda.gov/consumers/consumer-updates/spilling-beans-how-much-caffeine-too-much
- Mayo Clinic. (2022). Caffeine content for coffee, tea, soda and more. Retrieved from: https://www.mayoclinic.org/healthy-lifestyle/nutrition-and-healthy-eating/in-depth/caffeine/art-20049372
- University of Bath. “Drink coffee after breakfast, not before, for better metabolic control.” ScienceDaily. ScienceDaily, 2 October 2020. <www.sciencedaily.com/releases/2020/10/201002091053.htm>.
- Evans J, Richards JR, Battisti AS. Caffeine. [Updated 2024 May 29]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519490/
- Kline CE, Chasens ER, Bizhanova Z, Sereika SM, Buysse DJ, Imes CC, Kariuki JK, Mendez DD, Cajita MI, Rathbun SL, Burke LE. The association between sleep health and weight change during a 12-month behavioral weight loss intervention. Int J Obes (Lond). 2021 Mar;45(3):639-649. doi: 10.1038/s41366-020-00728-8. Epub 2021 Jan 7. PMID: 33414489; PMCID: PMC7914147.
- Humer E, Pieh C, Brandmayr G. Metabolomics in Sleep, Insomnia and Sleep Apnea. Int J Mol Sci. 2020 Sep 30;21(19):7244. doi: 10.3390/ijms21197244. PMID: 33008070; PMCID: PMC7583860.
Pelz, Mindy. Personal interview. September 7, 2023.
Hernandez, Adrian. Personal interview. October 5, 2024.