Long Story Short
- Sleep and the immune system have a synergistic relationship, meaning good sleep enhances immune function, while poor sleep can weaken it.
- An immune response to acute illness promotes sleep, which is why people who get sick need to answer their body’s call for rest.
- Lack of sleep can disrupt immune function, increasing the risk of infections and aggravating chronic inflammatory diseases. (1)
- Just one night of not getting enough sleep can lower the activity of your immune system’s natural killer cells and raise the levels of inflammation in your body. (2)
- One night of bad sleep won’t necessarily make you sick, but your suppressed immune system is more susceptible to becoming sick as a result.
- You are three times more likely to catch the common cold if you get less than seven hours of sleep on a regular basis. (3)
- Cancer risk is 69 percent higher in people who get less than seven hours of sleep on a regular basis. (4)
You may remember your mom saying if you went outside in the fall without a jacket, you would catch a cold. Now you might be telling your own kids that, or perhaps an equally persuasive threat about how they better go to bed if they want to avoid the flu.
But can a lack of sleep make you sick? Maybe — but it’s not that simple. We’re exploring the complex relationship between sleep and the immune system, including what you can do to improve both.
Note: The content on Sleepopolis is meant to be informative in nature, but it shouldn’t be taken as medical advice, and it shouldn’t take the place of medical advice and supervision from a trained professional. If you feel you may be suffering from any sleep disorder or medical condition, please see your healthcare provider immediately.
How the Immune System Works
Your immune system is a complex network of cells, tissues, and organs that work together — like your skin, spleen, lymph nodes, bone marrow, and tonsils — to protect you from harmful germs that can cause infections and illnesses. One of the most important factors in how well your immune defense system can do its job is getting enough restorative sleep. Sleep loss affects your immune system’s ability to both detect and respond to pathogens, so getting enough Zzz’s is vital to your immune system’s health. (5)
While you’re sleeping, your body makes and releases proteins that help coordinate your immune system’s surveillance and response. These proteins are called cytokines. They’re part of your body’s first line of defense against the damaging effects of infections, inflammation, and stress. But when you’re not getting enough quality sleep, your body can’t make as many of these important proteins. When cytokines are limited, so are your body’s immune defense mechanisms, leaving you more vulnerable to illness. (6)
Sleep also boosts the activity of T-cells, a type of white blood cell involved in recognizing and attacking infected or abnormal cells. T-cells rely on a process called adhesion, which allows them to latch onto infected cells and destroy them — a deadly hug, so to speak. Research shows that sleep deprivation makes it harder for T-cells to do this job. (7)
Finally, getting good sleep helps balance inflammation-promoting and inflammation-fighting responses in your body. This balance is important because it prevents your immune system from overreacting. (8)
Types of Immunity
Your body has two types of immunity, each of which carries out specific functions to help protect you from harm: innate and adaptive immunity. (9)(10)
We asked immunologist Nikky Contractor, PhD and R&D leader at Amway, to help us differentiate between these two arms that help keep you healthy:
Innate Immunity
The innate immune system is the body’s first line of defense against infections, which can be thought of as bacterial and viral “invaders.” The innate immune system is the body’s rapid response unit that surveys and reacts within minutes to the presence of an invader. The specialized cells of the innate immune system detect infectious agents early and send “danger” signals to the body to increase the inflammatory response, which in turn eliminates these invaders, explains Contractor.
Innate immunity provides a fast, non-specific response to pathogens, and involves your skin and mucus membranes in places like your nose, mouth, throat, and eyes. For example, that obnoxious runny nose and sore throat you get when you’re sick? They may make it harder to sleep (or breathe) but they’re an indication that your immune system is working to fight back. (9)
While these symptoms are usually the result of both the innate and adaptive immune responses working together to fight an infection, they’re more directly tied to the innate response, which is your body’s first line of defense against pathogens. (9)
This brings us to another question. If you have a virus like COVID-19 but aren’t experiencing the usual viral symptoms, does that mean your immune system isn’t working? Nope. Being asymptomatic can indicate that your immune system is effectively managing the threat, preventing it from causing noticeable symptoms. However, note that even if you’re asymptomatic (while having a positive COVID test) you can still be contagious. (11)(12)
Your innate immune system relies on quality sleep to produce cytokines so it can quickly and effectively respond to threats like inflammation and germs. Innate immunity works quickly and doesn’t remember past infections, so it reacts the same way to threats each time, even if you’ve faced them before. (13)
Adaptive Immunity
The adaptive immune system contains B cells, which produce antibodies, and T cells, which kill infected cells and conduct and refine the antibody response. Both of these cells have a specialized ability to recognize specific invaders, notes Contractor. In other words, they can tell the difference between an influenza virus and a hepatitis virus, and they develop targeted responses to fight each. (14)
In addition, while innate immune cells quickly forget the invader that they just met when the infection is cleared, adaptive immune cells have the ability to remember, enabling them to have a more rapid and amplified response the next time the same bacteria or virus is encountered, Contractor explained. (15)
While adaptive immunity doesn’t cause physical symptoms directly, the processes involved in this immune response can lead to symptoms like fever, swelling, redness, tiredness, and even a runny nose or sore throat. (14)
Our adaptive immunity requires healthy and sufficient sleep to do its job well and to help your body form long-term immunity. A lack of sleep, poor sleep quality, or irregular sleep patterns weaken adaptive immunity, which makes it harder to form strong immune memories after infections or vaccinations. (16)
How Sleep Affects the Immune System
How well your immune system can do its job is significantly affected by the quality, duration, and consistency of sleep you get.
According to Contractor, there’s a complex relationship between sleep and the immune system that’s regulated by circadian rhythms, hormones, and cytokines. She notes that research has shown that not getting enough sleep can lead to higher levels of inflammation in the body, lower activity of natural killer cells (a part of the immune system that fights off infections), and less production of antibodies (which help the body recognize and fight germs). (1)
In other words, sleep is a crucial component of a healthy, effective immune system. First, the different stages of sleep contribute to your immune function in unique ways: (17)
- Non-rapid eye movement (NREM) sleep: Your body makes immune cells, like T-cells and cytokines, to fight inflammation and infections, while also helping your body recover.
- Rapid eye movement (REM) sleep: This stage is essential for your brain to organize and consolidate memories, which indirectly benefits immunity by helping manage mood and stress.
Getting consistent, restorative sleep helps lower your risk of developing chronic diseases that can disrupt (and possibly shorten) your life. Quality sleep helps support healthy blood sugar management, improving insulin sensitivity and reducing your risk of type 2 diabetes. It also supports heart health by lowering inflammation, heart rate, stress responses, and blood pressure. (1)(18)
On top of all that, sleep helps control appetite-regulating hormones (like ghrelin and leptin) to support healthy weight management. (19) This matters because emerging evidence indicates that being overweight or obese is associated with a weakened immune system, demonstrated by the link between obesity and a wide range of complications with dysregulated immunity as an underlying factor. (20) Some research indicates that chronic sleep deprivation or irregular sleep patterns (such as with shift work) may also increase the risk of certain cancers because of how it impairs immune surveillance, which is the process by which your immune system watches for, detects, and ultimately destroys cancer cells. (21)(22)
Sleep also plays a vital role in the effectiveness of vaccines, like an annual flu shot. Vaccines work by stimulating your immune system to produce antibodies, which help your body recognize and fight off specific germs. Studies have shown that people who are well-rested produce more robust antibody responses to vaccines than those who are sleep-deprived. (23)
For example, research on the flu vaccine demonstrated that people who got a full night’s sleep before and after vaccination had higher antibody levels, improving their protection against the flu virus. (24) On the flip side, sleep deprivation (sleeping for 6 hours or less) around the time of vaccination can make it harder for your body to create enough antibodies, reducing how effective said vaccine is at offering protection. (25)
Finally, as mentioned, while you’re sleeping, your immune system is creating cytokine proteins and preparing immune cells for their jobs of identifying and destroying threats. This requires adequate, consistent sleep, and a lack of such rest can impair these immune processes — which brings us to another important question.
Can Lack of Sleep Make You Sick?
The interaction between sleep and the immune system is complex and has nuances experts are still trying to understand. “Nevertheless, it is clear that sleep deprivation can lead to increased susceptibility to infection and that adequate sleep can help to regulate healthy normal immune responses,” Contractor says. (1)
Lack of sleep can also slow your recovery time after you get sick. Contractor says that this is because when you’re not well-rested, your immune system suffers, leading to a compromised ability to fight infections — especially if you’re experiencing ongoing sleep deprivation. (18)
Chronically not getting enough sleep is associated with a higher risk of short-term common illnesses like colds and flu, as well as long-term conditions like cardiovascular disease and diabetes. This is because sleep is crucial for your body’s ability to regulate things like your blood pressure, blood sugar, and inflammatory response. (1)(18)
Other Effects of Sleep Deprivation
Your immune system isn’t the only thing that suffers when you’re not getting enough sleep. Think about the last time you were struggling to catch up on your rest and how it made you feel — probably not great.
Ongoing sleep deprivation can affect your mental and emotional health, making it harder to concentrate, make decisions, or remember things. Nobody feels good when they’re not well-rested and, as a result, a lack of sleep can make you more irritable, anxious, or stressed out. (26) Poor sleep also has a tendency to reduce good self-care activities, including regular exercise, engaging in meaningful social relationships, and tapping into creative pursuits.
Your body also suffers physically when it hasn’t properly recharged overnight. Sleep deprivation can disrupt normal metabolic functions, making you feel weak and fatigued. Ever noticed that you’re more likely to reach for a breakfast of donuts than oatmeal when you’re not sleeping well? That’s because sleep deprivation is also known to increase appetite, particularly for foods that are rich in simple, easily digested (and often sugary) carbohydrates and may not be the most nutrient-dense. (27)
Other long-term effects of ongoing sleep deprivation can include:
- Unintentional weight gain from disrupted appetite regulation or overeating (28)
- Impaired memory (29)
- Increased risk of mental health effects like anxiety and depression (30)
- Heart health effects like high blood pressure or high levels of fats in the blood (30)
How the Immune System Affects Sleep
Sleep and immunity are on a two-way street. Not only do your sleep habits influence your immune function, but your immune system can also affect your sleep. Here’s how.
First, let’s go back to those cytokine proteins we talked about before. Not only are they key players in your immune response, but they’re also involved in regulating your rest. Some cytokines, especially ones involved in inflammation, directly promote sleep.
According to Contractor, “Both bacterial and viral infections have been shown to cause an increase in particular phases of the sleep cycle during the course of an infection.” She notes that these changes may be related to bacterial or viral components that stimulate pro-inflammatory cytokine production.
When you’re sick, your body spends more time in the phase known as non-rapid eye movement (NREM) sleep, so it can recover, fight off germs, and repair its tissues. For example, if you have an infection, your immune system ramps up and increases cytokine production, enhancing your sleep. (17)
Next, your immune system also influences your propensity for sleep, AKA your circadian rhythm, which determines when you feel tired and when you feel awake. When you’re under the weather, your immune response alters this cycle to encourage more sleep — less wakefulness — to support healing. An activated immune system does what it needs to do in your body to get you feeling better as quickly as possible, including shifting your sleep patterns so you’re more inclined to rest. (31)
Callout? Though many of us don’t realize it, inflammation is closely tied to our immune systems. Short-term and targeted inflammation can be normal, but chronic inflammation is often a result of an immune system that’s out of whack. (32) That excessive inflammation in your body can promote a number of health problems, including trouble sleeping or even trouble staying awake. Inflammation can be triggered by a variety of factors — conditions like obesity or rheumatoid arthritis, for example, can trigger systemic (whole-body) inflammation, making it hard to sleep and even causing insomnia. This creates a vicious cycle where poor sleep can further aggravate your immune response, worsening inflammation. (33)
Finally, allergies are another example of immune-related issues that can interfere with sleep. Allergies are an overreaction of the immune system to substances that are recognized as “foreign”, like pollen, dust mites, pet dander, and mold. When you have symptoms like congestion, sneezing, and itchiness in your face and throat, it can be hard to fall and stay asleep, leading to tiredness during the day. (34)
How to Strengthen the Immune System
Strengthening your immune system is important to help it continue working properly to detect and protect you from harmful germs. Fortunately, you can support a healthy immune system through many everyday habits and lifestyle practices.
First, improving your sleep is essential. One of the best ways to do this is by putting intentional sleep hygiene practices into place. Sleep hygiene refers to the habits and practices that are conducive to sleeping well on a regular basis, which may include: (35)
- Following a consistent sleep-wake pattern, with consistent wake-up and bedtimes, to help regulate your body’s internal clock
- Creating a relaxing bedtime routine, such as reading, journaling, or stretching to help your body wind down before rest
- Ditching the use of screens, which are known to emit blue light that suppresses your brain’s ability to release melatonin, a hormone that helps make you sleepy in preparation for bedtime (36) On top of that, social media engagement, following the news, and some forms of entertainment can stir up emotions that are incompatible with sleep or effectively hypnotize you into staying awake longer than you intended.
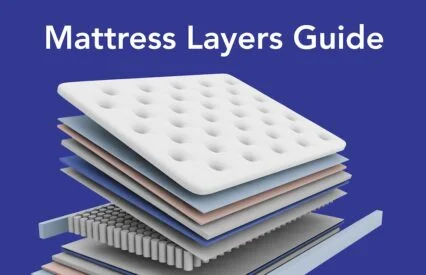
- Designing a sleep-promoting environment in your bedroom by keeping it dark, reducing excessive noise, and ensuring a supportive and comfortable mattress.
Sleep is a cornerstone of immune health, but it’s not the only factor involved in your immunity. Other healthy lifestyle practices that support a healthy immune system include:
- Proper nutrition: Optimizing the nutritional quality of your diet is essential for immune health. Boost your intake of unprocessed or minimally-processed foods, including fruits, vegetables, whole grains, nuts, seeds, legumes, and other lean proteins to ensure adequate intake of vitamins, minerals, fiber, and antioxidants that support immunity and wellness. (37)(38)
- Regular exercise: Moving your body daily promotes better circulation, which allows your immune cells to move around your body more efficiently. Not to mention, exercise is also important for lowering inflammation, protecting against chronic disease, supporting healthy weight management, and even boosting your mood. Moderate exercise is good, as some evidence suggests that when it becomes strenuous, it can actually reduce immunity. (39)(40)
- Stress management: We all feel the burdens of stress from time to time, but when it’s ongoing, it can weaken the immune system by increasing the production of cortisol, a hormone that suppresses immune response. Practicing stress-reducing activities like meditation, deep breathing, and exercise can help support your ability to fight off infections. (41)(42)
FAQs
How does sleep help when you’re sick?
Sleep helps the immune system function more efficiently by promoting the production of proteins that fight infection and inflammation (called cytokines). Restorative sleep also supports your body’s ability to recover by saving energy for healing processes, so you can feel better sooner.
Can staying up late make you sick?
While staying up too late once in a while isn’t going to make you sick, it can weaken your immune system. Ongoing sleep deprivation increases inflammation and reduces the production of infection-fighting cells and proteins, making your body more vulnerable to getting sick.
The Last Word From Sleepopolis
The relationship between your immune system and your sleep patterns is another great example of how interconnected our bodies are. Your immune system is tasked with protecting you from germs, and to do so, you need to support it with adequate sleep. Adopt good sleep hygiene habits along with lifestyle practices like improving your nutrition, exercise, and stress management.
Sources
- Garbarino S, Lanteri P, Bragazzi NL, Magnavita N, Scoditti E. Role of sleep deprivation in immune-related disease risk and outcomes. Commun Biol. 2021;4(1):1304. Published 2021 Nov 18. doi:10.1038/s42003-021-02825-4
- CDC.gov. (2020). NIOSH Training for Nurses on Shift Work and Long Work Hours. Retrieved from: https://www.cdc.gov/niosh/work-hour-training-for-nurses/longhours/mod2/05.html
- Yale Medicine. (2023). How Sleep Affects Your Immune System. Retrieved from: https://www.yalemedicine.org/news/how-sleep-affects-immunity
- Ning, D., Fang, Y., & Zhang, W. (2023). Association of habitual sleep duration and its trajectory with the risk of cancer according to sex and body mass index in a population-based cohort. Cancer, 129(22), 3582-3594. https://doi.org/10.1002/cncr.34951
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. In brief: What are the organs of the immune system? [Updated 2023 Aug 14]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279395/
- Liu C, Chu D, Kalantar-Zadeh K, George J, Young HA, Liu G. Cytokines: From Clinical Significance to Quantification. Adv Sci (Weinh). 2021;8(15):e2004433. doi:10.1002/advs.202004433
- Lin Y, He L, Cai Y, Wang X, Wang S, Li F. The role of circadian clock in regulating cell functions: implications for diseases. MedComm (2020). 2024;5(3):e504. Published 2024 Mar 11. doi:10.1002/mco2.504
- Dzierzewski JM, Donovan EK, Kay DB, Sannes TS, Bradbrook KE. Sleep Inconsistency and Markers of Inflammation. Front Neurol. 2020;11:1042. Published 2020 Sep 16. doi:10.3389/fneur.2020.01042
- InformedHealth.org [Internet]. Cologne, Germany: Institute for Quality and Efficiency in Health Care (IQWiG); 2006-. In brief: The innate and adaptive immune systems. [Updated 2023 Aug 14]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK279396/
- Johns Hopkins Medicine. The Immune System. Retrieved from: https://www.hopkinsmedicine.org/health/conditions-and-diseases/the-immune-system
- Boyton, R. J., & Altmann, D. M. (2021). The immunology of asymptomatic SARS-CoV-2 infection: What are the key questions? Nature Reviews Immunology, 21(12), 762-768. https://doi.org/10.1038/s41577-021-00631-x
- Sayampanathan AA, Heng CS, Pin PH, Pang J, Leong TY, Lee VJ. Infectivity of asymptomatic versus symptomatic COVID-19. Lancet. 2021;397(10269):93-94. doi:10.1016/S0140-6736(20)32651-9
- Kaur BP, Secord E. Innate Immunity. Pediatr Clin North Am. 2019;66(5):905-911. doi:10.1016/j.pcl.2019.06.011
- Catania LJ. The adaptive (aka “acquired”) immune system: from friend to foe. The Paradox of the Immune System. 2022;25-43. doi:10.1016/B978-0-323-95187-6.00006-6
- Sette A, Crotty S. Adaptive immunity to SARS-CoV-2 and COVID-19. Cell. 2021;184(4):861-880. doi:10.1016/j.cell.2021.01.007
- Chi H, Pepper M, Thomas PG. Principles and therapeutic applications of adaptive immunity. Cell. 2024;187(9):2052-2078. doi:10.1016/j.cell.2024.03.037
- Besedovsky L, Lange T, Haack M. The Sleep-Immune Crosstalk in Health and Disease. Physiol Rev. 2019;99(3):1325-1380. doi:10.1152/physrev.00010.2018
- Liew SC, Aung T. Sleep deprivation and its association with diseases- a review. Sleep Med. 2021;77:192-204. doi:10.1016/j.sleep.2020.07.048
- Lin J, Jiang Y, Wang G, et al. Associations of short sleep duration with appetite-regulating hormones and adipokines: A systematic review and meta-analysis. Obes Rev. 2020;21(11):e13051. doi:10.1111/obr.13051
- Shaikh SR, Beck MA, Alwarawrah Y, MacIver NJ. Emerging mechanisms of obesity-associated immune dysfunction. Nat Rev Endocrinol. 2024;20(3):136-148. doi:10.1038/s41574-023-00932-2
- Lanza G, Mogavero MP, Salemi M, Ferri R. The Triad of Sleep, Immunity, and Cancer: A Mediating Perspective. Cells. 2024;13(15):1246. Published 2024 Jul 24. doi:10.3390/cells13151246
- Yeo BSY, Koh JH, Shi BY, et al. The association between sleep quantity, insomnia and lung cancer risk – A systematic review and meta-analysis. Sleep Breath. Published online August 15, 2024. doi:10.1007/s11325-024-03092-3
- Quach HQ, Warner ND, Ovsyannikova IG, et al. Excessive daytime sleepiness is associated with impaired antibody response to influenza vaccination in older male adults. Front Cell Infect Microbiol. 2023;13:1229035. Published 2023 Dec 12. doi:10.3389/fcimb.2023.1229035
- Prather AA, Pressman SD, Miller GE, Cohen S. Temporal Links Between Self-Reported Sleep and Antibody Responses to the Influenza Vaccine. Int J Behav Med. 2021;28(1):151-158. doi:10.1007/s12529-020-09879-4
- Millman J. (2023). UCLA Health. Too little sleep could make vaccination less effective. Retrieved from: https://www.uclahealth.org/news/release/too-little-sleep-could-make-vaccination-less-effective
- Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Med Rev. 2021;60:101556. doi:10.1016/j.smrv.2021.101556
- Liu S, Wang X, Zheng Q, Gao L, Sun Q. Sleep Deprivation and Central Appetite Regulation. Nutrients. 2022;14(24):5196. Published 2022 Dec 7. doi:10.3390/nu14245196
- Papatriantafyllou E, Efthymiou D, Zoumbaneas E, Popescu CA, Vassilopoulou E. Sleep Deprivation: Effects on Weight Loss and Weight Loss Maintenance. Nutrients. 2022;14(8):1549. Published 2022 Apr 8. doi:10.3390/nu14081549
- Kim T, Kim S, Kang J, Kwon M, Lee SH. The Common Effects of Sleep Deprivation on Human Long-Term Memory and Cognitive Control Processes. Front Neurosci. 2022;16:883848. Published 2022 Jun 2. doi:10.3389/fnins.2022.883848
- Zheng, N. S., Annis, J., Master, H., Han, L., Gleichauf, K., Ching, J. H., Nasser, M., Coleman, P., Desine, S., Ruderfer, D. M., Hernandez, J., Schneider, L. D., & Brittain, E. L. (2024). Sleep patterns and risk of chronic disease as measured by long-term monitoring with commercial wearable devices in the All of Us Research Program. Nature Medicine, 30(9), 2648-2656. https://doi.org/10.1038/s41591-024-03155-8
- Waggoner SN. Circadian Rhythms in Immunity. Curr Allergy Asthma Rep. 2020;20(1):2. Published 2020 Jan 10. doi:10.1007/s11882-020-0896-9
- Pahwa R, Goyal A, Jialal I. Chronic Inflammation. In: StatPearls. Treasure Island (FL): StatPearls Publishing; August 7, 2023.
- Ballesio, A. (2023). Where does inflammation in insomnia come from? And does it matter for comorbidity? Sleep, 46(10). https://doi.org/10.1093/sleep/zsad223
- Liu J, Zhang X, Zhao Y, Wang Y. The association between allergic rhinitis and sleep: A systematic review and meta-analysis of observational studies. PLoS One. 2020;15(2):e0228533. Published 2020 Feb 13. doi:10.1371/journal.pone.0228533
- Baranwal N, Yu PK, Siegel NS. Sleep physiology, pathophysiology, and sleep hygiene. Prog Cardiovasc Dis. 2023;77:59-69. doi:10.1016/j.pcad.2023.02.005
- Silvani MI, Werder R, Perret C. The influence of blue light on sleep, performance and wellbeing in young adults: A systematic review. Front Physiol. 2022;13:943108. Published 2022 Aug 16. doi:10.3389/fphys.2022.943108
- Munteanu C, Schwartz B. The relationship between nutrition and the immune system. Front Nutr. 2022;9:1082500. Published 2022 Dec 8. doi:10.3389/fnut.2022.1082500
- Janciauskiene S. The Beneficial Effects of Antioxidants in Health And Diseases. Chronic Obstr Pulm Dis. 2020;7(3):182-202. doi:10.15326/jcopdf.7.3.2019.0152
- Scheffer DDL, Latini A. Exercise-induced immune system response: Anti-inflammatory status on peripheral and central organs. Biochim Biophys Acta Mol Basis Dis. 2020;1866(10):165823. doi:10.1016/j.bbadis.2020.165823
- Simpson RJ, Campbell JP, Gleeson M, et al. Can exercise affect immune function to increase susceptibility to infection?. Exerc Immunol Rev. 2020;26:8-22.
- Knezevic E, Nenic K, Milanovic V, Knezevic NN. The Role of Cortisol in Chronic Stress, Neurodegenerative Diseases, and Psychological Disorders. Cells. 2023;12(23):2726. Published 2023 Nov 29. doi:10.3390/cells12232726
- Ishikawa Y, Furuyashiki T. The impact of stress on immune systems and its relevance to mental illness. Neurosci Res. 2022;175:16-24. doi:10.1016/j.neures.2021.09.005
Contractor, Nikky. Personal interview. September 20, 2024.