Sleep Restriction Therapy (SRT) is a component of the Cognitive Behavioral Therapy for Insomnia (CBT-I) protocol, a type of therapy used to treat chronic insomnia lasting three months or longer. (1) Developed by psychologist and sleep specialist Arthur Spielman in the early 1980s, SRT can help to consolidate sleep by reducing the time spent in bed. (2)
Sleep restriction therapy is a natural, non-pharmaceutical treatment for chronic insomnia and is widely seen as an effective element of CBT-I. The focus of SCT is not on attempting to get more sleep, but on improving sleep efficiency and creating positive associations between the bed and sleep.
Sleep efficiency
The percentage of time spent sleeping while in bed. The number is calculated by dividing minutes spent asleep by minutes in bed. 85% or higher is considered healthy sleep efficiency.
Note: The content on Sleepopolis is meant to be informative in nature, but it shouldn’t take the place of medical advice and supervision from a trained professional. If you feel you may be suffering from any sleep disorder or medical condition, please see your healthcare provider immediately.
What is Sleep Restriction Therapy?
Sleep restriction therapy limits time in bed to the average number of hours actually spent sleeping. Many insomnia sufferers spend a significant amount of time trying to sleep, which reinforces negative psychological associations between the bed and insomnia. SRT conditions the body to sleep during a fixed amount of time without lying in bed awake or napping. (3)
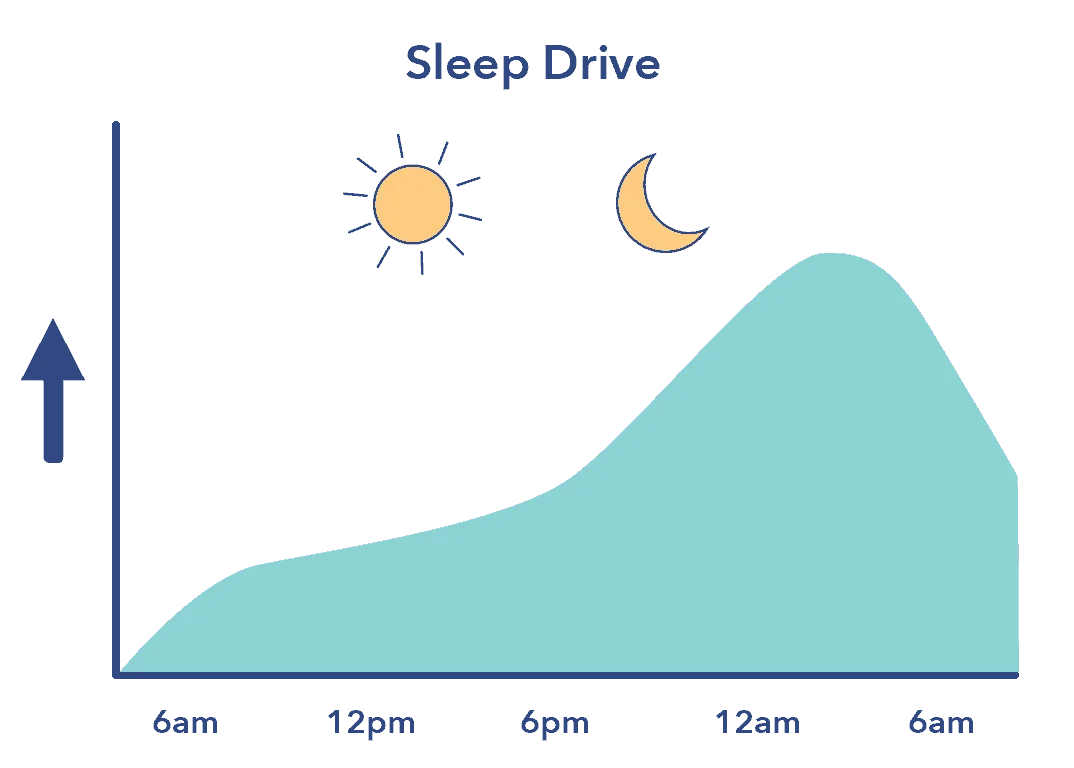
By reducing time in bed, the drive to sleep increases, improving the ability to fall asleep quickly without a long sleep latency period (time spent waiting to sleep).
SRT can improve sleep efficiency in the following ways:
- Sleep restriction not only reduces sleep latency, but increases the chance of sleeping through the night without waking.
- Due to its effect on sleep efficiency, SRT helps the brain develop a positive association between the bed and sleep.
- Foregoing naps further increases the sleep drive. (4)
- The consistent sleep and wake schedule of SRT helps to regulate the circadian rhythm and establish healthy sleep patterns.
Therapy protocol also encourages patients not to go to bed unless they’re sleepy, and to only use the bed for sleep and sex.
Practicing Sleep Restriction Therapy
SRT is typically undertaken with the supervision of a sleep specialist, in combination with other components of CBT-I such as stimulus control training. The essential elements of SRT are as follows:
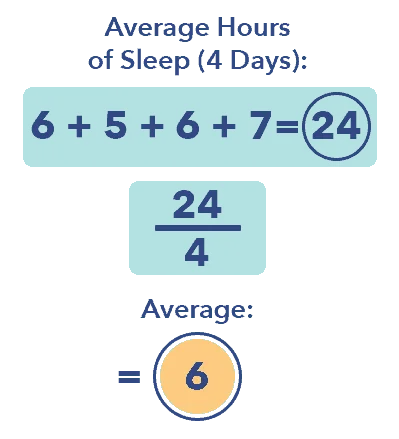
- The sleeper notes how much time they spend asleep over the course of several nights. The nightly average becomes the amount of time the sleeper is allowed to spend in bed. For example, if an insomnia sufferer typically spends 7 hours in bed, but sleeps only 6, SRT will begin with a period of six hours. Five and a half hours is the minimum amount of time a sleeper is permitted to spend in bed.
- Sleep and wake times are established and adhered to without exception. Sleep specialists typically recommend going to sleep later and waking at a normal time rather than going to bed and waking too early. A person who sleeps an average of six hours might go to sleep at 1 am and wake up at 7 am.
- During sleep restriction therapy, the sleeper does not take naps or deviate from the prescribed sleep period.
- Once the insomnia sufferer is able to sleep through the sleep period without lying awake. or waking during the night, time in bed increases gradually in increments of approximately 15 minutes
- The sleep period continues to increase until insomnia symptoms abate, sleep is consolidated, and daytime sleepiness is minimal. Sleep efficiency should be at 85%, meaning that 85% of time in bed is spent asleep. (5)
Though the principles of SRT may seem simple, they typically require discipline and commitment. Insomnia sufferers who are able to stick to the protocol usually notice improvements in sleep latency, nighttime waking, and sleep efficiency within the first week of treatment.
FAQ
Q: What is stimulus control therapy (SCT)? A: SCT helps to strengthen the association between the bed and sleep. Instructions include not looking at the clock while trying to sleep, and getting out of bed if not asleep within 20 minutes.Side Effects of Sleep Restriction Therapy
Because sleep restriction therapy rigorously controls the time spent in bed, it may lead to certain temporary side effects, including:
- Daytime sleepiness. The insomnia sufferer’s duration of sleep remains the same, so feelings of fatigue should not be greater than usual. Daytime sleepiness typically resolves as treatment continues and insomnia symptoms improve.
- Cognitive effects such as difficulties with focus, memory, and concentration. Again, these should be similar to the effects of sleep loss usually experienced by the insomnia sufferer.
- Circadian rhythm disruption due to a sudden change in sleep patterns.
- Increased feelings of anxiety and other emotions related to sleep difficulty. (6) Some insomniacs may rely on time in bed as a form of stress relief. Sleep restriction removes this time buffer and may temporarily increase anxiety.
In addition to these side effects, sleep restriction therapy may also frustrate insomnia sufferers who are accustomed to lying awake in bed rather than engaging in other activities. The feeling of needing to find something to do with extra hours at night and in the morning may make adhering to the protocol more difficult for some people.
Circadian rhythm
The 24-hour cycle that controls sleep and other physiological functions in all living beings.
Sleep Compression Therapy
Sleep compression therapy is similar to sleep restriction therapy in that the goal of treatment is to reduce time spent lying awake in bed. Sleep compression therapy is more gradual than SRT, and is typically recommended for people who sleep fairly well, but still experience time awake in bed as well as mild daytime sleepiness. (7)
A candidate for sleep compression therapy might be someone who sleeps seven hours on average, but spends eight hours in bed. They feel mildly fatigued on seven hours of sleep, and want to feel more alert and rested. Sleep compression therapy entails the following:
- Estimate average time spent in bed.
- Reduce time in bed gradually, by approximately 20 minutes each week. (8)
- Continue as long as daytime sleepiness or other indications of sleep loss don’t increase.
- Once daytime sleepiness increases, the sleeper’s reached their limit! Sleep should be efficient and consolidated, and fixed boundaries for sleeping and waking should be established to maintain healthy sleep patterns.
Because the principles of sleep compression are so gradual, they’re generally easier to follow than those of sleep restriction. Time in bed is decreased by approximately three minutes per day, which may help mitigate such side effects as daytime sleepiness and anxiety.
Last Word from Sleepopolis
Sleep restriction therapy and sleep compression therapy are two of the most commonly used treatments for insomnia, particularly when symptoms continue for three months or longer. Insomnia sufferers may notice an improvement in as little as a week.
Sleep restriction involves rapid changes that take discipline and commitment, but may be the best choice for treating persistent sleep difficulties. Sleep compression is often used in milder cases of insomnia, or when a person who experiences no or only mild daytime impairment from sleep loss wants to reduce their time in bed. Both are non-drug treatments that are generally considered by sleep specialists to be safe and effective, particularly when undertaken in combination with other components of cognitive behavioral therapy for insomnia.
References
- Falloon K, Elley CR, Fernando A 3rd, Lee AC, Arroll B., Simplified sleep restriction for insomnia in general practice: a randomised controlled trial, British Journal of General Practice, Aug. 2015
- Arthur J. Spielman, Treatment of Chronic Insomnia by Restriction of Time in Bed, Sleep, Jan. 1987
- McDevitt EA, Alaynick WA, Mednick SC., The effect of nap frequency on daytime sleep architecture, Physiology&Behavior, Aug. 2012
- Reed DL, Sacco WP. Measuring Sleep Efficiency: What Should the Denominator Be?, Journal of Clinical Sleep Medicine, Feb. 15, 2016
- Goldstein AN, Greer SM, Saletin JM, Harvey AG, Nitschke JB, Walker MP., Tired and Apprehensive: Anxiety Amplifies the Impact of Sleep Loss on Aversive Brain Anticipation, The Journal of Neuroscience, June 26, 2013
- Kenneth L. Lichstein, S. Justin Thomas, Sleep Compression, BSM Treatment Protocols for Insomnia, June 26, 2013
- Lichstein, Kenneth L., Relaxation and sleep compression for late-life insomnia: A placebo-controlled trial, Journal of Consulting and Clinical Psychology, 2001

























