The word insomnia is often used to describe any form of trouble sleeping. Insomnia can mean nearly anything — trouble falling asleep for a single night, trouble staying asleep for a few weeks, or difficulty falling back to sleep for several months.
What does insomnia really refer to? Does it have a single, defined meaning, or can the term insomnia be applied broadly, as it often is? What’s the difference between short-term insomnia and insomnia as a sleep disorder?
Insomnia
From the Latin insomnis, meaning sleepless. Insomnia is difficulty falling asleep, staying asleep, or falling back to sleep.
Note: The content on Sleepopolis is meant to be informative in nature, but it shouldn’t take the place of medical advice and supervision from a trained professional. If you feel you may be suffering from any sleep disorder or medical condition, please see your healthcare provider immediately.
What is Insomnia?
Insomnia is the world’s most common sleep disorder. (1) Depending on how the term is applied, up to 30% of people have insomnia at any given time. If the diagnosis of insomnia requires that the sleeper feel impaired during the day due to lack of sleep, then the number drops to 10%. Eliminate people with symptoms lasting less than one month, or whose symptoms can’t be explained by a psychiatric or medical condition, and the number drops even further, to 6%. (2)
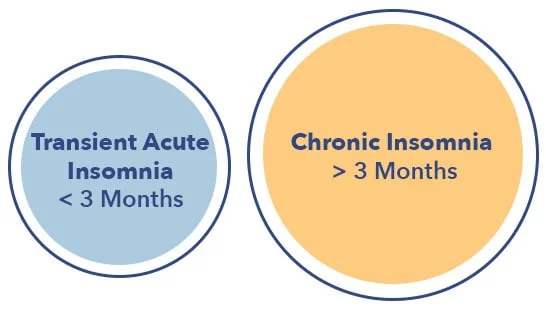
Insomnia is split into two main categories: transient acute and chronic. Transient acute insomnia lasts less than three months, while chronic insomnia persists for three months or longer. (3)
Transient Acute Insomnia
Transient acute insomnia differs from insomnia disorder in duration and cause. Transient acute insomnia can last for a single day or several weeks. (4)
Symptoms of Transient Acute Insomnia
Symptoms of transient acute insomnia are common, and include some or all of the following criteria:
- Difficulty falling asleep
- Difficulty staying asleep
- Difficulty falling back to sleep
- Daytime impairment due to lack of sleep
- Nonrestorative or poor quality sleep
Transient acute insomnia may occur while attempting to fall asleep, during the night, or near morning.
These three stages are referred to as onset, maintenance, and late insomnia. (5) No matter when it occurs during the night, transient acute insomnia may result in a wide range of effects, such as:
- Feeling tired and/or groggy upon waking up
- Daytime fatigue
- Irritability or mood swings
- Difficulty concentrating
- Trouble retaining new information
- Reduced coordination
- Increased risk of errors and accidents at home or on the job
- Diminished work performance
- Trouble engaging in social activities
FAQ
Q: How does insomnia cause memory problems? A: Memories are consolidated and stored during sleep. Without sufficient sleep, this process is interrupted or slowed.Transient Acute Insomnia Causes
Causes of transient insomnia symptoms are varied, and often associated with psychological or lifestyle factors. (6) Causes include:
- Stress
- Anxiety
- Depression
- Significant life changes such as a move, new job or school, or divorce
- Grief
- Chronic pain
- Alcohol, medication, or drug consumption
- Jet lag or daylight saving time
Diagnosing Insomnia
The diagnosis of both transient and chronic insomnia usually requires a sleep history, but rarely requires a sleep study or additional testing. In addition to a history of symptoms, a doctor may:
- Suggest you keep a sleep diary to track your sleep patterns and identify factors that might contribute to your insomnia issues
- Ask you to take one or several insomnia tests to better understand your sleep habits. These might include questionnaires such as the Insomnia Severity Index or a mental health examination
- Ask about your sleep habits and social environment
Treatment of Transient Acute Insomnia
Transient acute insomnia tends to be short-lived, and usually resolves on its own without medical or psychological treatment. (7) Symptoms may be relieved by practicing good sleep hygiene and/or addressing the underlying cause or stressor. Sleep medications might be prescribed to help the transient insomnia sufferer sleep during a difficult or painful period. Reassurance from a sleep specialist or psychotherapist may be enough to help alleviate symptoms or make them more tolerable.
Sleep hygiene
Sleep hygiene is a set of habits and practices intended to improve sleep.
Insomnia Disorder
Insomnia disorder, also known as chronic insomnia, is defined as difficulty falling asleep, staying asleep, or falling back to sleep for three months, at least three days a week. Chronic insomnia can last for years and may begin in childhood.
Insomnia Disorder Symptoms
Symptoms and effects of insomnia disorder are similar to transient acute insomnia, and are not typically relieved by lifestyle changes. Medications may offer some relief, but are not a long-term solution.
Insomnia Disorder Causes
Insomnia disorder is not generally associated with temporary circumstances or life stressors. The disorder nearly always has a single cause: negative psychological associations with the bed and sleep.
Insomnia disorder may begin with a bout of transient acute insomnia. Habits such as clock-watching and worrying that develop during a short-term episode of transient insomnia can turn into negative conditioning related to the sleeping environment and any attempt to sleep.
Even bedtime routines such as showering and brushing teeth can provoke the anxiety associated with being unable to fall asleep. (8) This conditioning may become chronic, and persist despite attempts to go to sleep earlier or improve sleep hygiene.

Insomnia Disorder Treatment
The most effective and proven treatment for insomnia disorder is cognitive behavioral therapy for insomnia, or CBT-I. This multi-component protocol includes stimulus control training, sleep restriction therapy, relaxation training, and cognitive behavioral therapy. (9)
The goal of stimulus control therapy is to create positive psychological associations between the bed and sleep, while sleep restriction limits time in bed to the average number of hours spent sleeping. Relaxation training utilizes such tools as mindfulness, yoga, guided imagery, and progressive muscle relaxation, while the cognitive behavioral element of therapy challenges dysfunctional beliefs and attitudes about sleep that may be contributing to chronic insomnia.
FAQ
Q: What is guided imagery? A: A stress management technique that might utilize visualization, music, vocal guidance, and self-hypnosis.Insomnia and Mental Health
Both transient and chronic insomnia are strongly associated with depression and other mood disorders. The inability to sleep is a common sign of many mood disturbances, including:
- Depression. Difficulty sleeping is often one of the first symptoms of depression. Research shows that acute insomnia is frequently related to the first onset of depression symptoms (10)
- Schizophrenia
- Social phobia
- Both the depressive and manic phases of bipolar disorder
- Post-traumatic stress disorder. Disrupted sleep and nightmares are common symptoms of post-traumatic stress disorder. Fear, hypervigilance, and paranoia may make sleep difficult or impossible. Insomnia may be caused by flashbacks, as well as hallucinations and talking or shouting during sleep
Insomnia is not only a symptom of depression and other mood disorders, it may be a cause. Studies reveal that insomnia can have serious and deleterious effects on the brain, making depression and anxiety more likely. Treating insomnia early may help prevent depression, just as treating depression may help prevent chronic insomnia.
Last Word from Sleepopolis
Though insomnia has become an umbrella term for any inability to sleep, transient acute insomnia and chronic insomnia are distinct sleep disturbances with different causes. Transient acute insomnia typically has a short course and resolves without medical treatment. Chronic insomnia lasts longer than three months and may be associated with mood disorders such as depression and anxiety.
While time is often the best remedy for transient acute insomnia, insomnia disorder is effectively treated by cognitive behavioral therapy for insomnia. CBT-I works remarkably well for the majority of chronic insomnia sufferers, reducing the need for medications and other less effective and enduring treatments.
References
- Bhaskar S, Hemavathy D, Prasad S., Prevalence of chronic insomnia in adult patients and its correlation with medical comorbidities, Journal of Family Medicine and Primary Care, Oct-Dec, 2016
- Roth T., Insomnia: Definition, Prevalence, Etiology, and Consequences, Journal of Clinical Sleep Medicine, Aug. 15, 2007
- Chien‐Ming Yang, Shih‐Chun Lin, Chung‐Ping Cheng, Transient Insomnia Versus Chronic Insomnia: A Comparison Study of Sleep‐Related Psychological/Behavioral Characteristics, Journal of Clinical Psychology, June 24, 2013
- Jason G. Ellis, Acute insomnia: Current conceptualizations and future directions, Sleep Medicine Reviews, Feb. 2012
- Ohayon MM., Nocturnal awakenings and comorbid disorders in the American general population, Journal of Psychiatric Research, Nov. 2008
- Ohayon MM, Lemoine P., A connection between insomnia and psychiatric disorders in the French general population, Encephale, Sep-Oct. 2002
- Kalyanakrishnan MD, Scheid MD, Treatment Options for Insomnia, American Family Physician, Aug. 15, 2007
- Sharma MP, Andrade C., Behavioral interventions for insomnia: Theory and practice, Indian Journal of Psychiatry, Oct-Dec. 2012
- Simon D. Kyle, Towards standardisation and improved understanding of sleep restriction therapy for insomnia disorder: A systematic examination of CBT-I trial content, Sleep Medicine Reviews, Feb. 2015
- Ellis JG, Perlis ML, Bastien CH, Gardani M, Espie CA., The Natural History of Insomnia: Acute Insomnia and First-onset Depression, Sleep, Jan. 1, 2014

























