Long Story Short
- Sleep and depression have a bidirectional relationship, meaning that while sleep can worsen depressive symptoms, depression can also affect sleep quality. (1)
- An average of 12 percent of U.S. adults experience depression in their lifetime. (2)
- About 75 percent of depression patients have issues falling asleep or staying asleep. (3)
- People with insomnia have a 10 times greater risk of developing depression than those who do not have this sleep disorder. (3)
- Improving your sleep can be a key step in managing depression. (3) (4)
Depression and sleep woes can come as a package deal: depression can steal your sleep, and missing out on your Zzzs can make depressive symptoms worse. Because their connection is so strong, treatment for one can also help the other, with the best treatments addressing both. (1) Below, we’ll explain the dance between depression and sleep and give you some tips to get better sleep with this mental health condition.
Note: The content on Sleepopolis is meant to be informative in nature, but it shouldn’t be taken as medical advice, and it shouldn’t take the place of medical advice and supervision from a trained professional. If you feel you may be suffering from any sleep disorder or medical condition, please see your healthcare provider immediately.
Understanding Depression
Depression, a common mood disorder, can change the way you think, feel, and live your daily life. When you have depression, simple things like eating, taking care of yourself, and sleeping can feel challenging. Experts divide depression into a few types, many of which fall under the category of “major depression.” (5)
Major depression affects 8.3 percent of U.S. adults and causes a low mood that interferes with daily activities on most days for at least two weeks. (6)
Perinatal depression (including postpartum depression), can happen anytime during pregnancy or in the months after childbirth. It affects 8.5 to 11 percent of pregnant women and 6.5 to 12.9 of women in the first year after a baby’s birth. (8)
Seasonal affective disorder (SAD) also falls under the umbrella of major depression and comes and goes with the seasons, usually beginning in the fall or winter and subsiding in the spring and summer. Anywhere from one to 10 percent of people can experience SAD, depending on where they live. (9)
Persistent depressive disorder is like major depression, but more rare (2.5 percent of U.S. adults) with milder symptoms that last longer — at least two years. (7)
Occasionally, depression can come with severe symptoms like hallucinations, but most types involve similar symptoms and treatments. (5)
Depression Causes, Symptoms and Treatments
To help you sleep better with depression, we first need to explain some depression basics. Once you know about depression causes, symptoms, and treatments, you can better understand how to incorporate the sleep tips we’ll offer.
Causes of Depression
Depression’s causes can depend on its type, but experts think — in combination with environmental factors — it may partly arise due to a mixup in brain chemicals (neurotransmitters) like serotonin and dopamine. These chemical messengers help regulate your mood, and when they aren’t released correctly it could cause depressive symptoms. (10)
Otherwise, the causes and risk factors of depression can vary quite a lot depending on the type of depression and the person experiencing it. With that in mind, here are some potential depression causes and risk factors: (5)
- Trauma: Traumatic events — especially those experienced at an early age — can cause brain changes that may make depression more likely later in life.
- Family members with depression: If a close family member has depression, you may be up to three times more likely to develop it yourself. (11)
- Life position and events: Marriage status, relationships, and financial situation can all contribute to depression’s development. (12)
- Medical conditions: If you have a chronic illness, including a mental health or sleep disorder, you may be at a higher risk for depression.
- Alcohol and drugs: If you overuse alcohol or use recreational drugs, your depression risk may increase. (13)
Symptoms of Depression
Some symptoms of depression may seem obvious, while others might surprise you. Depressive symptoms can include: (5)
- Feelings of sadness, anxiety, and emptiness
- Irritability, hopelessness, or restlessness
- Lower interest in hobbies, social withdrawal
- Difficulty sleeping or oversleeping
- Fatigue, and trouble concentrating during the day
- Appetite and weight changes
- Headaches and digestive issues
- Change in sexual desire
- Thoughts of self-harm or suicide
Get Help Now
If you are having thoughts of self-harm or suicide, you can call or text 988 to speak with someone right away at no cost.
Treatments for Depression
When you get a depression diagnosis, your provider may recommend one type of treatment or a combination. Some common depression treatments include:
Evidence-Based Psychotherapy
Also called “talk therapy” or “counseling,” psychotherapy is done with a mental health professional trained to help you identify thought patterns and behavior that feed your depression. Your provider may use a treatment called cognitive-behavioral therapy (CBT) — which is also used for insomnia — to retrain negative thought patterns. (5) (14) (15)
Medications
Many depression medications target those chemical brain messengers that aren’t working quite right. These meds can help correct the imbalance and diminish or resolve depressive symptoms. Some common medication types for depression include: (11)
- Selective serotonin reuptake inhibitors (SSRIs) like fluoxetine (Prozac) and sertraline (Zoloft)
- Tricyclic antidepressants (TCAs) like amitriptyline (Elavil) and doxepin (Silenor)
- Monoamine oxidase inhibitors (MAOIs) like isocarboxazid (Marplan) and phenelzine (Nardil)
- The serotonin antagonist and reuptake inhibitor, trazadone (16)
Brain Stimulation Therapy
If talk therapy and medications don’t cut it, providers may turn to brain stimulation therapies, which deliver a small amount of electricity to the brain through electrodes on the scalp or magnetic fields near your head. The electricity may promote positive brain activity and dampen harmful brain pathways. (5)
Light Therapy
Although not FDA approved, some people find shining a very bright light nearby for 30 minutes in the morning can help improve depressive symptoms in seasonal affective disorder, and possibly in other forms of depression. (5) (18)
Now that you know the basics of depression, we can talk about how it affects your sleep and how to boost your snoozing.
The Connection Between Depression and Sleep
Sleep and depression tend to feed off each other in a cycle because they are partly regulated by the same area of the brain: the hypothalamus, says Dr. Ilene Rosen, M.D., past president of the American Academy of Sleep Medicine and associate professor of medicine at the Perelman School of Medicine at the University of Pennsylvania. (1) Depression can change the way your brain gets you ready for sleep, and sleep disorders and deprivation can pave the way for depressive symptoms. (1)
The Sleep-Depression Loop
Depression and sleep problems often intertwine, with each amplifying the other, says Kristie Tse, a psychotherapist who treats depression. “From my work with clients, I’ve observed that when someone is feeling depressed, they often struggle with sleep — whether it’s difficulty falling asleep, staying asleep, or waking up too early,” says Tse.
This can lead to a restless cycle that can leave you exhausted during the day and deepen depression symptoms — which can then lead to even worse sleep the following night, Tse adds. (1) “I’ve worked with clients who, due to their depressive state, spiral into a cycle of negative thinking at night, making rest feel impossible,” says Tse. But by addressing both issues simultaneously, she has seen significant improvements in her clients’ mood and overall functioning.
Sleep Stages, Melatonin, and Circadian Rhythm
Research has found that people with depression often experience changes in rapid-eye movement (REM) sleep and restorative slow-wave sleep (SWS). (19) As the deepest non-REM sleep stage, SWS helps you feel rested the next day and also plays a big part in storing memories. (20)
The Sleep Stages
Once we fall asleep, we sleep in different stages: (21)
- N1 (light sleep)
- N2 (deeper sleep)
- N3 (deepest non-REM sleep, also known as slow wave sleep)
- REM (rapid-eye movement sleep)
How fast you can fall asleep is important, too, and some research suggests that people with depression have lower levels of melatonin — a hormone that signals to your brain that it’s time to get sleepy. (22) Melatonin also has a close relationship with your circadian rhythm, or internal clock, which helps manage your sleep and wake times. (23) Circadian rhythm disruption is common in mental health disorders like depression. (22)
Common Sleep Problems Associated With Depression
Depression can affect your sleep in more ways than one, but the most common sleep disorder with depression is insomnia: trouble falling asleep or staying asleep more than three nights a week for over three months. (24) In fact, the presence of insomnia can help diagnose depression. (1)
Less commonly, people with depression can also experience hypersomnia, in which you sleep all night, but then also feel like sleeping all day. (5) (25) (26) Hypersomnia may be more common with SAD or bipolar disorder — periods of euphoria or mania followed by depression. (27)
These sleep disorders are also common with depression: (19)
- Sleep disordered breathing: Issues with breathing around sleep, such as sleep apnea, in which your breathing pauses repeatedly while you snooze. (28) (29)
- Narcolepsy: Extreme daytime sleepiness with episodes of falling asleep unexpectedly throughout the day. (30)
- Restless legs syndrome (RLS): Uncomfortable sensations in your legs with a strong urge to move them for relief. (31)
Now that we’re up to speed on the basics, let’s talk about how to get better sleep when you have depression.
Tips For Sleeping Better With Depression
For those with depression, better sleep is possible through establishing good habits not only around bedtime, but throughout your day. “Getting better sleep while dealing with depression can be challenging, but there are several strategies that can help,” says Rosen.
Cue Your Brain with Routine
“To improve sleep when dealing with depression, I suggest establishing a consistent bedtime routine,” says Tse. A consistent routine signals to your brain that it’s time to wind down, and offers some stability surrounding bedtime, agrees Rosen, who adds, “If someone is having trouble setting these restrictions, they should first focus on setting a wake-up time.” (32)
Practice Calming Mindfulness
Depression symptoms can feel stressful, especially as bedtime approaches. To combat these feelings, you can try meditation and calming techniques as you prepare for bed, says Tse. Research results are mixed, but meditation and deep breathing may help you chill out before you try to sleep. (33) “[Wind down time] can reduce anxiety and stress, which often contribute to insomnia,” says Rosen.
Get Good at Sleep Hygiene
Sleep hygiene describes the various habits you have around sleep. (34) For example, good hygiene asks you to avoid screens before bed (their blue light can confuse your body into thinking it’s still time to party). “By reducing screen time by at least 30 minutes to an hour before bed, you allow your body to produce melatonin naturally, helping you fall asleep more easily,” says Rosen. (35) Good sleep hygiene also means steering clear of alcohol and tobacco close to bedtime, as they can mess with your sleep stages. (36) (37) (38)
Squeeze in Daily Exercise
Exercise boosts your mood and squashes stress — both key factors in helping you sleep, says Rosen. You don’t have to run a marathon — every bit of physical activity can help you sleep better that night. (39) “Regular exercise also tires the body, making it easier to fall asleep at night,” says Rosen, who recommends not exercising too close to bedtime, as you may find it harder to wind down for sleep. (40)
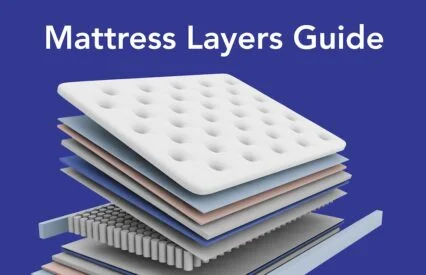
Keep it Comfy
“Create a comfortable sleep environment by making your bedroom dark, quiet, and cool,” says Tse. If you’re feeling depression symptoms approaching bedtime, a lumpy mattress with scratchy sheets may not call to you. Create your perfect combination with the best mattress, snuggly bedding, and supportive pillow to help you get in the sleepy groove. (41)
When To See A Doctor
If you think you may have depression, it’s important to reach out to a healthcare provider, especially if your symptoms don’t seem to be going anywhere and if they affect your day-to-day function or sleep. “I’ve seen clients who delay this step, believing they can handle it on their own, but they often find their situation worsening,” says Tse. (3)
Rosen agrees, saying, “If difficulties with falling asleep, staying asleep or waking up too early start to impact your daily life — affecting work, relationships or your ability to handle everyday tasks — it may be time to reach out to your healthcare provider or a psychiatrist.”
You never have to take on these feelings alone. Give your healthcare provider a call with any new depressive symptoms, and if you are in a mental health crisis or have thoughts of self-harm or suicide, call 911 or the national crisis line at 988 for immediate help.
FAQs
Is oversleeping a sign of depression?
In some cases, depression can cause hypersomnia, which makes you excessively sleepy during the day, even when you slept all night. (5) (25) (26) But, hypersomnia is rarer, and may be more common with SAD or bipolar depression. (27)
Do you need more sleep when you’re depressed?
Because depression affects your sleep stages and steals your deep sleep, you may feel like you need more sleep each day. (19)
Can depression lead to sleep disorders?
About 90 percent of people with depression also experience sleep disorders like insomnia, narcolepsy, sleep disordered breathing (including sleep apnea), and restless leg syndrome (RLS). (19)
The Last Word From Sleepopolis
Depression and sleep can often work against one another, but if you can break that cycle of worsening symptoms and snoozing, you can start feeling (and sleeping) better.
If you stick to a consistent routine, follow excellent sleep hygiene, get some exercise in the day, and turn your sleeping space into a cozy oasis, you may find sleep comes easier with depression. When in doubt, let your provider know what’s going on and they can help guide you to better snoozing!
Sources
- Riemann D, Krone LB, Wulff K, Nissen C. Sleep, insomnia, and depression. Neuropsychopharmacology. 2020;45(1):74-89. doi:10.1038/s41386-019-0411-y
- Major Depressive Disorder – StatPearls – NCBI Bookshelf. Accessed September 21, 2024. https://www.ncbi.nlm.nih.gov/books/NBK559078/
- Depression and Sleep: Understanding the Connection | Johns Hopkins Medicine. Accessed September 14, 2024. https://www.hopkinsmedicine.org/health/wellness-and-prevention/depression-and-sleep-understanding-the-connection
- Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Medicine Reviews. 2021;60:101556. doi:10.1016/j.smrv.2021.101556
- Depression | NAMI. Accessed September 14, 2024. https://www.nami.org/about-mental-illness/mental-health-conditions/depression/
- Major Depression – National Institute of Mental Health (NIMH). Accessed September 14, 2024. https://www.nimh.nih.gov/health/statistics/major-depression
- Persistent Depressive Disorder (Dysthymic Disorder) – National Institute of Mental Health (NIMH). Accessed September 14, 2024. https://www.nimh.nih.gov/health/statistics/persistent-depressive-disorder-dysthymic-disorder
- Dagher RK, Bruckheim HE, Colpe LJ, Edwards E, White DB. Perinatal Depression: Challenges and Opportunities. J Womens Health (Larchmt). 2021;30(2):154-159. doi:10.1089/jwh.2020.8862
- Seasonal Affective Disorder – StatPearls – NCBI Bookshelf. Accessed September 14, 2024. https://www.ncbi.nlm.nih.gov/books/NBK568745/
- Jiang Y, Zou D, Li Y, et al. Monoamine Neurotransmitters Control Basic Emotions and Affect Major Depressive Disorders. Pharmaceuticals. 2022;15(10):1203. doi:10.3390/ph15101203
- Depression – StatPearls – NCBI Bookshelf. Accessed September 14, 2024. https://www.ncbi.nlm.nih.gov/books/NBK430847/
- Curran E, Rosato M, Ferry F, Leavey G. Prevalence and factors associated with anxiety and depression in older adults: Gender differences in psychosocial indicators. Journal of Affective Disorders. 2020;267:114-122. doi:10.1016/j.jad.2020.02.018
- Depression & Substance Abuse Treatment Plans, Medication, Therapy. Accessed September 22, 2024. https://americanaddictioncenters.org/co-occurring-disorders/depressive-disorders
- Gautam M, Tripathi A, Deshmukh D, Gaur M. Cognitive Behavioral Therapy for Depression. Indian J Psychiatry. 2020;62(Suppl 2):S223-S229. doi:10.4103/psychiatry.IndianJPsychiatry_772_19
- Walker J, Muench A, Perlis ML, Vargas I. Cognitive Behavioral Therapy for Insomnia (CBT-I): A Primer. Klin Spec Psihol. 2022;11(2):123-137. doi:10.17759/cpse.2022110208
- Trazodone: MedlinePlus Drug Information. Accessed September 22, 2024. https://medlineplus.gov/druginfo/meds/a681038.html
- Brain Stimulation Therapies – National Institute of Mental Health (NIMH). Accessed September 17, 2024. https://www.nimh.nih.gov/health/topics/brain-stimulation-therapies/brain-stimulation-therapies
- Light therapy: Not just for seasonal depression? – Harvard Health. Accessed September 17, 2024. https://www.health.harvard.edu/blog/light-therapy-not-just-for-seasonal-depression-202210282840
- Fang H, Tu S, Sheng J, Shao A. Depression in sleep disturbance: A review on a bidirectional relationship, mechanisms and treatment. J Cell Mol Med. 2019;23(4):2324-2332. doi:10.1111/jcmm.14170
- Zhang Y, Gruber R. Can Slow-Wave Sleep Enhancement Improve Memory? A Review of Current Approaches and Cognitive Outcomes. Yale J Biol Med. 2019;92(1):63-80.
- Patel AK, Reddy V, Shumway KR, Araujo JF. Physiology, Sleep Stages. In: StatPearls. StatPearls Publishing; 2023. Accessed January 6, 2024. http://www.ncbi.nlm.nih.gov/books/NBK526132/
- Pandi-Perumal SR, Monti JM, Burman D, et al. Clarifying the role of sleep in depression: A narrative review. Psychiatry Research. 2020;291:113239. doi:10.1016/j.psychres.2020.113239
- Physiology, Circadian Rhythm – StatPearls – NCBI Bookshelf. Accessed January 14, 2024. https://www.ncbi.nlm.nih.gov/books/NBK519507/
- Insomnia – What Is Insomnia? | NHLBI, NIH. Accessed September 14, 2023. https://www.nhlbi.nih.gov/health/insomnia
- Hypersomnia | National Institute of Neurological Disorders and Stroke. Accessed September 14, 2023. https://www.ninds.nih.gov/health-information/disorders/hypersomnia
- Idiopathic Hypersomnia – StatPearls – NCBI Bookshelf. Accessed September 14, 2024. https://www.ncbi.nlm.nih.gov/books/NBK585065/
- Murru A, Guiso G, Barbuti M, et al. The implications of hypersomnia in the context of major depression: Results from a large, international, observational study. European Neuropsychopharmacology. 2019;29(4):471-481. doi:10.1016/j.euroneuro.2019.02.011
- Sleep Apnea – What Is Sleep Apnea? | NHLBI, NIH. Accessed November 20, 2023. https://www.nhlbi.nih.gov/health/sleep-apnea
- Chen CM, Kuo CY, Wu MN, Hung JY, Hsu CY, Tsai MJ. Increased risk of major depressive disorder in sleep apnea patients in Taiwan. Sci Rep. 2021;11(1):765. doi:10.1038/s41598-020-80759-3
- Narcolepsy – Narcolepsy | NHLBI, NIH. Accessed September 14, 2023. https://www.nhlbi.nih.gov/health/narcolepsy#
- Restless Legs Syndrome | National Institute of Neurological Disorders and Stroke. Accessed May 6, 2024. https://www.ninds.nih.gov/health-information/disorders/restless-legs-syndrome
- Chaput JP, Dutil C, Featherstone R, et al. Sleep timing, sleep consistency, and health in adults: a systematic review. Appl Physiol Nutr Metab. 2020;45(10 (Suppl. 2)):S232-S247. doi:10.1139/apnm-2020-0032
- Peters AL, Saunders WJ, Jackson ML. Mindfulness-Based Strategies for Improving Sleep in People with Psychiatric Disorders. Curr Psychiatry Rep. 2022;24(11):645-660. doi:10.1007/s11920-022-01370-z
- Baranwal N, Yu PK, Siegel NS. Sleep physiology, pathophysiology, and sleep hygiene. Progress in Cardiovascular Diseases. 2023;77:59-69. doi:10.1016/j.pcad.2023.02.005
- Silvani MI, Werder R, Perret C. The influence of blue light on sleep, performance and wellbeing in young adults: A systematic review. Front Physiol. 2022;13:943108. doi:10.3389/fphys.2022.943108
- Ben Salah A, Nakajima M, DeAngelis BN, al’Absi M. Effects of tobacco addiction on links between early life adversities, sleep disturbance, and depression: A moderated mediation approach. Prev Med Rep. 2020;20:101225. doi:10.1016/j.pmedr.2020.101225
- Guan T, Zhang C, Zou X, et al. The Influence of Alcohol Consumption, Depressive Symptoms and Sleep Duration on Cognition: Results from the China Health and Retirement Longitudinal Study. Int J Environ Res Public Health. 2022;19(19):12574. doi:10.3390/ijerph191912574
- He S, Hasler BP, Chakravorty S. Alcohol and sleep-related problems. Current Opinion in Psychology. 2019;30:117-122. doi:10.1016/j.copsyc.2019.03.007
- Brupbacher G, Gerger H, Zander-Schellenberg T, et al. The effects of exercise on sleep in unipolar depression: A systematic review and network meta-analysis. Sleep Med Rev. 2021;59:101452. doi:10.1016/j.smrv.2021.101452
- Physical Activity May Lessen Depression Symptoms | NIH News in Health. Accessed September 14, 2024. https://newsinhealth.nih.gov/2019/03/physical-activity-may-lessen-depression-symptoms
- 5 Sleep Tips that Can Help with Depression | NAMI: National Alliance on Mental Illness. Accessed September 14, 2024. https://www.nami.org/complimentary-health-approaches/5-sleep-tips-that-can-help-with-depression/
Tse, Kristie. Personal Interview. September 11, 2024.
Rosen, Ilene, MD. Personal Interview. September 13, 2024.