Fibromyalgia makes you more sensitive to pain, which you may feel all over your body. (1) About four million adults in the U.S. have fibromyalgia syndrome (FMS), and women make up 80 to 90 percent of those diagnosed. (1) (2)
This condition can also cause other health problems, including sleep disruption. (1) “[In fibromyalgia], sleep is disrupted because any type of pain will disrupt sleep,” says Dr. Aly Cohen, MD, integrative rheumatologist based in Princeton, New Jersey. Not only can pain steal sleep, missing sleep can make pain feel worse. (3)
While that may sound like a whole lot of bad news, we have some tips for you to get your best sleep with fibromyalgia. But first, let’s talk about how and why fibromyalgia disturbs your snoozing.
Note: The content on Sleepopolis is meant to be informative in nature, but it shouldn’t be taken as medical advice, and it shouldn’t take the place of medical advice and supervision from a trained professional. If you feel you may be suffering from any sleep disorder or medical condition, please see your healthcare provider immediately.
Long Story Short
- Fibromyalgia can upset sleep by increasing your perception of pain, disrupting your sleep structure, and putting you at higher risk for mental issues that also steal sleep.
- Some common sleep disorders that come alongside fibromyalgia include insomnia, restless leg syndrome, and sleep apnea.
- You may improve your sleep despite fibromyalgia by practicing good sleep hygiene, mindfulness, cutting out cigarettes, adjusting your sleeping positions, and more.
How Fibromyalgia Impacts Sleep
A huge proportion of people (90 percent!) with fibromyalgia report trouble sleeping or poor sleep quality, especially when their FMS symptoms get severe. (4) Let’s look at why.
Sleep Structure
All adults go through four stages of sleep (not including wakefulness), from light to deep sleep. (5) During your nightly snooze-a-thon, you move in and out of these stages, each of which has unique characteristics and different jobs to do. (6)
The Four Sleep Stages
- N1/Light sleep is the first of three non-rapid eye movement (NREM) sleep stages.
- N2/Deeper sleep gives your brain a chance to consolidate memories from the day.
- In N3/Deepest non-REM sleep, your body repairs and regrows damaged tissue and builds up your immune system.
- REM/rapid-eye movement sleep claims most of your dreaming time. (5)
When you have fibromyalgia, though, these sleep stage patterns can get disrupted. (7) That’s why, even though many with FMS say they get a full eight hours of sleep, they also complain of trouble falling asleep, staying asleep, and daytime fatigue. (4)
Pain
As Cohen said earlier, pain can ruin anyone’s rest, and pain from fibromyalgia can be a big risk factor for sleep challenges. Along with heightened pain perception, those with FMS may have low growth hormone, which typically helps the body repair microtrauma. (4)
Additionally if your sleep gets disrupted often your body can’t heal itself as well, which may lead to more pain and sleeplessness. (4) This can read as bleak, but it’s worth noting that research into fibromyalgia is ongoing, and there are some doctor-approved tips below to help you combat some of the challenges that come along with FMS.
Mental Health
Mental health disorders like depression and anxiety don’t get along with sleep even in people without fibromyalgia. (8) But when you add this condition into the mix, they can each make the other worse. (9)
In one large study review, researchers found that over 60 percent of people with fibromyalgia experience depression in their lifetimes. (10) People with FMS pain report more depressive symptoms and less sleep, even when they spend more time in bed. (4)
But hang in there! We have a few sleep disorders to cover and then we’ll get into some sleep tips for anyone with fibromyalgia.
Fibromyalgia and Sleep Disorders
Fibromyalgia symptoms can make it hard to sleep, and sometimes FMS can also come hand in hand with diagnosable sleep disorders. (4)
Insomnia and Fibromyalgia
About one third of the global population has insomnia, which means you have trouble falling asleep, staying asleep all night, and getting good quality rest for three or more nights a week, over a period of three months or more. (11) (12)
Insomnia has a strong connection with fibromyalgia: over 50 percent of people with FMS experience insomnia chronically. (13)
Restless Leg Syndrome and Fibromyalgia
Restless leg syndrome (RLS) causes an uncomfortable sensation in your legs that gives you a powerful urge to move them for relief. These symptoms often worsen at night and are a hallmark sleep disorder for people with fibromyalgia. (14) In fact, one study found people with RLS were almost twice as likely to also have fibromyalgia than those without RLS. (15)
Sleep Apnea and Fibromyalgia
Sleep apnea, a condition that pauses your breathing through the night, can also be more common in people with fibromyalgia. (16) Research tells us those with FMS are more likely to have a higher body weight, which can also put you at a higher risk for sleep apnea. (4)
One study review found 85 percent of people with FMS seen at a sleep clinic were diagnosed with obstructive sleep apnea, and ultimately the authors recommend sleep studies for anyone with fibromyalgia. (16)
You made it through the heavier reading about the how and why behind the relationship between fibromyalgia and sleep — now it’s time for some tips.
Sleep Tips for People with Fibromyalgia
Sleep tips can look similar for people with a wide variety of health issues. For example, sleep hygiene can help most people sleep better, including those with FMS. (17) (18) But we have honed and polished our sleep tips for fibromyalgia, tailored to bring you the most relief and get the best sleep possible.
Prep for Bed
When Cohen talks to her patients with fibromyalgia about better sleep, she recommends focusing on the prep. Sleeping may have felt easy at some point in your life, but you eventually have to work for it, she says.
To prepare for good sleep, Cohen suggests planning your social life around your sleep needs and steering clear of technology before bed, in addition to the tips below.
Practice Mindfulness
Mindfulness can describe a fairly long list of relaxing practices. When you focus on your senses and feelings for a moment or two, you’re practicing mindfulness. It can also include deep breathing techniques, guided imagery, and relaxation exercises. (19)
Although small, studies about mindfulness on sleep in fibromyalgia have found some encouraging results: better sleep and less pain. (20) (21) Mindfulness may work best in FMS when you practice it frequently. (22)
Try Cognitive Behavioral Therapy for Insomnia (CBT-I)
Cognitive behavioral therapy for insomnia (CBT-I), a method used to combat insomnia in people of all health backgrounds, can help improve sleep, pain, anxiety, and depression in those with fibromyalgia. (4)
By using provider-led pain education, thought re-training, and sleep hygiene training, CBT-I has helped plenty of people with FMS improve their nightly rest. (4)
Exercise Often
When you have FMS, the more you exercise and the less time you spend sitting or lying down during the day, the better you should be able to control your pain and improve your sleep. (4)
Cardiovascular fitness training may work best for fibromyalgia, and experts recommend a minimum of 30 minutes of aerobic exercise (that elevates your heart rate) three times a week. (18) Resistance training (with weights) and aquatic exercise have also led to better sleep for people with FMS. (4)
Cut Out Tobacco
Smoking can make you feel worse — especially when you have fibromyalgia — by causing more pain, which may lead to worse sleep. (23) This habit can also boost your risk for cognitive dysfunction with FMS, which means you could begin to have trouble with attention, memory, planning, and learning. (24) (25)
If you’re ready to quit, you don’t have to do it alone: the Centers for Disease Control (CDC) offers a long list of free resources to help you start on the path toward a smoke-free life. (26)
Find Your Sweet Spot for Sleeping Positions
When you live with chronic pain, it’s important to sleep in a supported position, especially if you like to sleep on your side. (27) If you’re a side-sleeper, be sure you keep your knees even with each other, adding a pillow in between. Prefer your back for snoozing? Try bending your knees over a pillow to keep the perfect curve in your back and relax those muscles. (28)
Ask About Medications
Some antidepressants like amitriptyline (Elavil) and duloxetine (Cymbalta) help lower pain and improve sleep for people with FMS. (4) Nerve medications like gabapentin (Neurontin) have also shown the same effects, plus better slow-wave (very deep) sleep and less anxiety and depression. (4) (29)
Zolpidem (Ambien) and other sleeping pills may work to help you sleep better in the short term, but most practitioners caution against using sleep aids like this longer than a few weeks as they could become habit-forming. (30)
Use Wet Heat
Lots of people use a hot pack for sore muscles, but wet heat may work best if you have FMS. “Wet heat gets into muscle, which is where a lot of the pain originates from in fibromyalgia,” says Cohen. (31)
She says you can even take a regular heating pad and surround it with a wet towel for optimal effects. Cohen recommends hot baths with Epsom salt for its magnesium-fueled pain-relieving effects. (4) (32)
Consider Alternative Treatments
Chamomile works great to get you ready for bed, says Cohen, who suggests magnesium glycinate supplements to her patients with fibromyalgia to quiet their mind and improve pain.
Melatonin supplements may work well for some people with FMS by improving symptoms stemming from low sleep quality, like fatigue and pain. (4) Experts have found that boosting vitamin D may help lessen your symptoms, so adding this micronutrient to your daily supplements or getting some extra sun in the afternoon may also help improve your sleep. (22) (33)
As with all medications and supplements, be sure to check in with your healthcare provider before you start taking anything new.
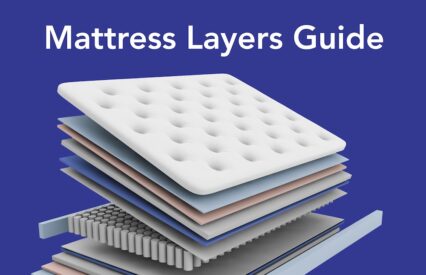
The Best Bedding for People with Fibromyalgia
When fibromyalgia pain tries to disrupt your sleep, your mattress may make or break your beauty rest. For all chronic pain, medium-firm mattresses have proven the most effective for less discomfort and better sleep quality. (34)
You can peruse our sleep expert-approved mattresses for fibromyalgia and pick one that suits your needs. But your mattress isn’t alone in helping you sleep better with fibromyalgia — your pillow plays an important role, too.
You may need to try a few pillows out to find your perfect fit, but its height should feel just right and support your neck, keeping it in line with the rest of your spine. (28) (35) “A good pillow can offset a bad mattress — and it’s cheaper and easier to return,” adds Cohen.
FAQs
Why is it so hard to sleep with fibromyalgia?
Does lying down make fibromyalgia worse?
Experts don’t say lying down makes fibromyalgia worse, but restless leg syndrome — one common sleep disorder that comes with FMS — can get worse when you sit or lie down. (36)
How do you get a good night’s sleep with fibromyalgia?
The Last Word From Sleepopolis
If chronic fibromyalgia pain and bad sleep has you down, we’ve got you. While we can’t fix all your medical woes, we can give you our tips for your best sleep ever with fibromyalgia. Give our suggestions a try, but remember that it’s important to work with your healthcare provider. They can help you make a plan, rule out anything else going on, and help you take more steps on the path to your best rest.
Sources
- Fibromyalgia | CDC. Accessed June 8, 2024. https://www.cdc.gov/arthritis/types/fibromyalgia.htm
- Climent-Sanz C, Morera-Amenós G, Bellon F, et al. Poor Sleep Quality Experience and Self-Management Strategies in Fibromyalgia: A Qualitative Metasynthesis. J Clin Med. 2020;9(12):4000. doi:10.3390/jcm9124000
- Haack M, Simpson N, Sethna N, Kaur S, Mullington J. Sleep deficiency and chronic pain: potential underlying mechanisms and clinical implications. Neuropsychopharmacology. 2020;45(1):205-216. doi:10.1038/s41386-019-0439-z
- OBM Neurobiology | Sleep Dysfunction in Fibromyalgia and Therapeutic Approach Options. Accessed June 8, 2024. https://www.lidsen.com/journals/neurobiology/neurobiology-04-01-049
- Patel AK, Reddy V, Shumway KR, Araujo JF. Physiology, Sleep Stages. In: StatPearls. StatPearls Publishing; 2023. Accessed January 6, 2024. http://www.ncbi.nlm.nih.gov/books/NBK526132/
- Sleep Physiology – Sleep Disorders and Sleep Deprivation – NCBI Bookshelf. Accessed June 8, 2024. https://www.ncbi.nlm.nih.gov/books/NBK19956/
- Duo L, Yu X, Hu R, Duan X, Zhou J, Wang K. Sleep disorders in chronic pain and its neurochemical mechanisms: a narrative review. Front Psychiatry. 2023;14:1157790. doi:10.3389/fpsyt.2023.1157790
- Oh CM, Kim HY, Na HK, Cho KH, Chu MK. The Effect of Anxiety and Depression on Sleep Quality of Individuals With High Risk for Insomnia: A Population-Based Study. Front Neurol. 2019;10:849. doi:10.3389/fneur.2019.00849
- Zhao SS, Holmes MV, Alam U. Disentangling the relationship between depression and chronic widespread pain: A Mendelian randomisation study. Seminars in Arthritis and Rheumatism. 2023;60:152188. doi:10.1016/j.semarthrit.2023.152188
- Yepez D, Grandes XA, Talanki Manjunatha R, Habib S, Sangaraju SL. Fibromyalgia and Depression: A Literature Review of Their Shared Aspects. Cureus. 14(5):e24909. doi:10.7759/cureus.24909
- Roth T. Insomnia: Definition, Prevalence, Etiology, and Consequences. Journal of Clinical Sleep Medicine. 2019;3(5 suppl):S7-S10. doi:10.5664/jcsm.26929
- Insomnia – What Is Insomnia? | NHLBI, NIH. Accessed September 14, 2023. https://www.nhlbi.nih.gov/health/insomnia
- McCrae CS, Curtis AF, Kay DB. The clinical neuroscience of the insomnia–fibromyalgia link: An overview for clinicians. In: Overlapping Pain and Psychiatric Syndromes: Global Perspectives. Oxford University Press; 2020:203-220. doi:10.1093/med/9780190248253.003.0015
- Restless Legs Syndrome – StatPearls – NCBI Bookshelf. Accessed June 8, 2024. https://www.ncbi.nlm.nih.gov/books/NBK430878/
- Alzabibi MA, Shibani M, Alsuliman T, et al. Fibromyalgia: epidemiology and risk factors, a population-based case-control study in Damascus, Syria. BMC Rheumatol. 2022;6:62. doi:10.1186/s41927-022-00294-8
- Meresh ES, Artin H, Joyce C, et al. Obstructive sleep apnea co-morbidity in patients with fibromyalgia: a single-center retrospective analysis and literature review. Open Access Rheumatol. 2019;11:103-109. doi:10.2147/OARRR.S196576
- Espie CA. The ‘5 principles’ of good sleep health. Journal of Sleep Research. 2022;31(3):e13502. doi:10.1111/jsr.13502
- Fibromyalgia – StatPearls – NCBI Bookshelf. Accessed June 8, 2024. https://www.ncbi.nlm.nih.gov/books/NBK540974/
- Mindfulness exercises – Mayo Clinic. Accessed May 10, 2024. https://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/mindfulness-exercises/art-20046356
- Park M, Zhang Y, Price LL, Bannuru RR, Wang C. Mindfulness is associated with sleep quality among patients with fibromyalgia. Int J Rheum Dis. 2020;23(3):294-301. doi:10.1111/1756-185X.13756
- Gordon S, Brown R, Hogan M, Menzies V. Mindfulness as a Symptom Management Strategy for Fibromyalgia: An Integrative Review. J Holist Nurs. 2023;41(2):200-214. doi:10.1177/08980101221123833
- Fibromyalgia: In Depth | NCCIH. Accessed June 8, 2024. https://www.nccih.nih.gov/health/fibromyalgia-in-depth
- Croghan IT, Hurt RT, Ganesh R, et al. The Association of Current Tobacco Status With Pain and Symptom Severity in Fibromyalgia Patients. mcp:iqo. 2021;5(3):614-624. doi:10.1016/j.mayocpiqo.2021.03.008
- Ge L, D’Souza RS, Oh T, et al. Tobacco Use in Fibromyalgia Is Associated With Cognitive Dysfunction. Mayo Clin Proc Innov Qual Outcomes. 2019;3(1):78-85. doi:10.1016/j.mayocpiqo.2018.12.002
- Dhakal A, Bobrin BD. Cognitive Deficits. In: StatPearls. StatPearls Publishing; 2023. Accessed January 12, 2024. http://www.ncbi.nlm.nih.gov/books/NBK559052/
- How to Quit Smoking | Quit Smoking | Tips From Former Smokers | CDC. Accessed June 8, 2024. https://www.cdc.gov/tobacco/campaign/tips/quit-smoking/index.html
- Cary D, Jacques A, Briffa K. Examining relationships between sleep posture, waking spinal symptoms and quality of sleep: A cross sectional study. PLoS One. 2021;16(11):e0260582. doi:10.1371/journal.pone.0260582
- Sleeping positions that reduce back pain – Mayo Clinic. Accessed June 8, 2024. https://www.mayoclinic.org/diseases-conditions/back-pain/in-depth/sleeping-positions/art-20546852
- Fibromyalgia | FMS | MedlinePlus. Accessed June 8, 2024. https://medlineplus.gov/fibromyalgia.html
- Zolpidem: MedlinePlus Drug Information. Accessed October 10, 2023. https://medlineplus.gov/druginfo/meds/a693025.html#side-effects
- Cao CF, Ma KL, Li QL, et al. Balneotherapy for Fibromyalgia Syndrome: A Systematic Review and Meta-Analysis. J Clin Med. 2021;10(7):1493. doi:10.3390/jcm10071493
- Shin HJ, Na HS, Do SH. Magnesium and Pain. Nutrients. 2020;12(8):2184. doi:10.3390/nu12082184
- Ümit YALÇIN1, , Sevtap Badıl GÜLOĞLU. Effects of Vitamin D on Pain Severity, Quality of Life, Depression and Sleep in Patients with Fibromyalgia. Akdeniz Medical Journal. Published online April 3, 2021.
- Authors, Barbara AM, Grobelna A. Therapeutic Mattresses for Chronic Pain: CADTH Health Technology Review. Canadian Agency for Drugs and Technologies in Health; 2022. Accessed June 1, 2024. http://www.ncbi.nlm.nih.gov/books/NBK599022/
- Yamada S, Hoshi T, Toda M, Tsuge T, Matsudaira K, Oka H. Changes in neck pain and somatic symptoms before and after the adjustment of the pillow height. J Phys Ther Sci. 2023;35(2):106-113. doi:10.1589/jpts.35.106
- Restless legs syndrome – Symptoms and causes. Mayo Clinic. Accessed June 4, 2024. https://www.mayoclinic.org/diseases-conditions/restless-legs-syndrome/symptoms-causes/syc-20377168
Aly Cohen, MD. Personal Interview. May 25, 2024.