For some people, nights aren’t a time of relaxation, but of restlessness, strange sensations, and even pain.
These are the symptoms experienced by sufferers of Restless Legs Syndrome, or RLS. RLS is a sensory and motor disorder that can impact a person’s ability to fall asleep, stay asleep, or remain still for extended periods of time.
Also known as Willis-Ekbom Disease, Restless Legs Syndrome is considered both a neurological disorder and a sleep disorder. The condition causes uncomfortable sensations in the limbs, as well as an overwhelming urge to move in an attempt to gain relief from those sensations.
RLS affects approximately 8% of the population in the United States, though this number may be low due to under-diagnosis. The disorder is not fatal, but can have a profound affect on sleep, health, and quality of life. (1)
Note: The content on Sleepopolis is meant to be informative in nature, but it shouldn’t taken as medical advice, and it shouldn’t take the place of medical advice and supervision from a trained professional. If you feel you may be suffering from any sleep disorder or medical condition, please see your healthcare provider immediately.
Symptoms of Restless Legs Syndrome
Because RLS follows a circadian rhythm, symptoms of discomfort and restlessness commonly worsen at night, disrupting an affected person’s ability to fall and/or stay asleep.
Cases of Restless Legs Syndrome are generally classified as either primary or idiopathic, or secondary. (2) In primary or idiopathic RLS, the cause of the disorder is unknown.
Primary RLS is more common than the secondary form, and is typically associated with a positive family history of the disorder. In secondary RLS, the condition is often provoked by another medical condition, drug, or vitamin/mineral deficiency. Secondary RLS may resolve when the precipitating disorder is treated.
Both the primary and secondary forms of Restless Legs Syndrome are characterized by the following symptoms:
- An uncomfortable feeling in the legs that may be described as itchy, throbbing, achy, crawling, pulling, or similar to pins and needles or electric shocks. The sensations can occur on one or both sides of the body, or alternate between the two sides. Less commonly, the feeling of discomfort may occur in the feet, arms (3), chest, or head
- A powerful urge to move the legs in an effort to reduce the uncomfortable sensations associated with the disorder
- Moving or stretching the limbs temporarily relieves the symptoms, which return when movement is stopped
- Symptoms worsen in the evening and when the afflicted person is lying or sitting for extended periods of time. The sensations may occur during a long car or plane ride, while watching a movie, or while lying in bed

What Causes Restless Legs Syndrome?
Though the exact mechanism behind RLS is unclear, it is likely caused by a combination of genetic and environmental factors. Some of these factors include:
- Dopamine dysfunction. There is strong evidence to suggest that RLS may result from an imbalance of dopamine, a brain chemical involved in regulating muscle movement as well as reward, attention, and memory. Disruption of dopamine pathways may result in the involuntary movements that are characteristic of RLS (4)
- Iron deficiency. Though the effective use of drugs that act on dopamine indicates a strong connection between dopamine and RLS, lack of iron in the brain may also play a significant role in the disorder. Levels of iron in the blood of RLS patients frequently appear normal, but are insufficient in the brain. Any condition that lowers available iron in the body increases the risk of RLS (5)
- Genetics. As many as 50% of people who suffer from primary Restless Legs Syndrome have a family member with the condition. This statistic supports the theory that genes play a prominent role in development of the disorder (6)
- Nighttime worsening of RLS symptoms may suggest a connection to the release of melatonin (7), a hormone released by the pineal gland in the brain in preparation for sleep

RLS symptoms may be triggered or worsened by certain drugs and conditions, including:
- Some antidepressants, anti-nausea drugs, antipsychotic drugs, calcium channel blockers, and cold and allergy medications containing antihistamines, which may block the brain’s dopamine receptors (8)
- Vitamin or mineral deficiencies. Magnesium and vitamin B-12 deficiency may have a link to the condition
- Pregnancy. (9) Some women experience symptoms of Restless Legs Syndrome during pregnancy, particularly during the last trimester. If RLS is triggered by pregnancy, most women will experience relief from symptoms within a month of delivery
- Sleep deprivation. RLS may cause sleep deprivation, and sleep deprivation may in turn provoke symptoms of RLS
- Alcohol, caffeine, and/or nicotine
RLS Fact: There may be an association between RLS and Attention Deficit/Hyperactivity Disorder, another neurological condition that involves the dysfunction of dopamine, an essential neurotransmitter (10)
In addition to medications and genetic and environmental factors, serious medical disorders may worsen or trigger RLS. Genetics may also be implicated in the connection between RLS and certain medical conditions, including:
- Diabetes
- End-stage renal disease
- Fibromyalgia
- Lyme disease
- Stroke (11)
- Multiple sclerosis (MS)
- Parkinson’s Disease
- Peripheral neuropathy (nerve damage)
- Rheumatoid arthritis
- Narcolepsy

When RLS is associated with narcolepsy, the cause is less likely to be genetic. Symptoms of RLS tend to appear approximately ten years after narcolepsy diagnosis. (12)
How Is Restless Legs Syndrome Diagnosed?
There is currently no specific medical test for RLS. Because diagnosis depends in part on a patient’s reporting of symptoms, RLS may frequently be under-diagnosed. (13) A clinical diagnosis of Restless Legs Syndrome requires that all of the following criteria be met:
- Uncomfortable sensations in the limbs, along with a strong impulse to move the legs
- Restlessness that results in such activities as pacing, massaging the limbs, or tossing and turning in bed
- Symptoms occur or worsen while at rest and are relieved by activity
- Symptoms increase in number and severity in the evening and at night
During an evaluation of RLS symptoms, a doctor may ask about family and medical history, other medical conditions, daytime sleepiness and other sleep information, and medication use. A sleep study may be ordered, as well as a blood test to check levels of iron in the blood.
A doctor will not diagnose RLS if sensory symptoms and restlessness begin while walking. Symptoms of the disorder must begin at rest to qualify as Restless Legs Syndrome.
Who Is At Risk for Restless Legs Syndrome?
Though RLS can occur at any time of life, the average age at diagnosis is forty-six. A third of sufferers are twenty years old or younger when diagnosed with the disorder. Some RLS sufferers experience their first symptoms before the age of ten.

Particular genetic and environmental factors make a diagnosis of RLS more likely. (14) People at risk for Restless Legs Syndrome include:
- Those with a family history of RLS. Because RLS has a strong genetic component, the risk of RLS for those with an affected family member may be as high as 50% (15)
- Sufferers of certain neurological movement disorders such as Parkinson’s Disease or Multiple Sclerosis (16)
- People taking medications or using substances known to exacerbate RLS, such as antidepressants
- Someone who has abnormal dopamine and/or iron levels in the brain
- Pregnant women, especially those in the final trimester
Additionally, there are other factors that may increase the risk of RLS:
- Female gender. RLS tends to be more common in women (17)
- Advancing age. RLS can affect people of any age, but is most common in those middle-aged or older
- Northern European descent
RLS Fact: Other disorders may cause symptoms similar to those experienced by RLS sufferers, including akathisia, which causes a feeling of inner restlessness, most often in the legs. Akathisia is not associated with sleeping, however, and is most commonly caused by anti-psychotic medications
Early-Onset Vs. Late-Onset RLS
RLS that begins before age 45 is considered early-onset. RLS after 45 is late-onset. Early-onset RLS may begin in the teenage years or earlier, and typically has a strong genetic component. Late-onset RLS occurs in middle age, and is often a secondary condition caused by other medical issues, medications, or nervous system disorders.
The early-onset form of RLS tends to affect women more often than men. In this type of RLS, the sensations in the limbs are not usually painful. Signs of insufficient sleep may be some of the first symptoms, particularly in children. Sensory symptoms may be dismissed by parents and doctors as growing pains.
Early-onset RLS may begin gradually and persist for a lifetime. (18) Daily symptoms might not appear for decades. The course of the disorder may also be more severe in early-onset RLS, though remission is possible, and can result in months or even years of relief.
Those diagnosed with late-onset RLS do not usually have a family history of the disease, and may experience painful as well as uncomfortable sensations in the limbs. Late-onset RLS is usually a secondary disorder triggered or caused by another medical condition or medication. The late-onset form of the disease may resolve with successful treatment of the underlying condition.
The Sensations of RLS: Paresthesias and Dysesthesias
The uncomfortable sensations characteristic of RLS are divided into two categories: Paresthesias and Dysethesias.
Paresthesias are sensations that are not generally considered painful, such as tingling, chill feelings, prickling, or numbness. Dysethesias are usually felt to be painful, and include burning, unrelieved itching, pins and needles, and electric shock sensations.

The paresthesias and dysethesias of RLS do not typically occur on the skin, but are felt to come from within the limb itself. Movement often helps to relieve the discomfort of paresthesias and dysethesias, prompting some sufferers to pace or keep the legs continually in motion.
The sensations of RLS can range from mild to severe, and are often unpredictable. They may change from day to day, or come and go. Some people experience symptoms only occasionally, while others suffer from them every night.
Paresthesias and dysethesias may also be symptoms of other disorders, such as peripheral neuropathy, multiple sclerosis, diabetes, and fibromyalgia.
Periodic Limb Movements in Sleep and RLS
RLS often occurs in conjunction with other irregular movements called Periodic Limb Movements in Sleep, or PLMS. More than 80% of people with RLS may have PMLS, as well.
PMLS is characterized by repetitive movements of the lower limbs and feet, including twitching, kicking, flexing and extension of the toes, and bending of the knees and ankles. Sudden jerking may awaken those afflicted, or cause partial awakenings that result in poor quality sleep. (19)
PMLS differs from Periodic Limb Movement Disorder, which does not occur secondary to another sleep disorder such as RLS. Periodic Limb Movements in Sleep are common in the general population and in people with RLS, while Periodic Limb Movement Disorder is rare.
The movements of PMLS occur during the lighter stages of non-REM sleep, when dreaming is absent, however they can also occur during waking hours. The jerking and other movements of PMLS may occur every 20 to 30 seconds throughout the night.
PLMS does not occur during REM sleep because of the muscle paralysis characteristic of this stage of sleep. The exception to this may be when PLMS occurs in people with REM Sleep Behavior Disorder, in which the normal paralysis of REM sleep is absent.
PMLS is also common in narcolepsy sufferers, those with abnormal sleep/wake patterns such as shift workers, and people withdrawing from the benzodiazepine class of drugs, such as Valium. Certain substances may exacerbate PMLS, including some antidepressants and caffeine. Stress and sleep deprivation may also cause worsening of symptoms.
Due to its effect on sleep, PLMS may cause daytime sleepiness and other signs of poor-quality sleep, including depression and reduced ability to concentrate. In addition, PLMS and RLS may both be implicated in the development of cardiovascular disease and hypertension. (20)
How Does Restless Legs Syndrome Impact Sleep?
Because RLS symptoms get worse at night, sufferers often find it difficult to fall and stay asleep. (21) RLS tends to occur during early stages of sleep, increasing the risk of sleep-onset insomnia and/or frequent awakening before deep sleep has occurred.
People with moderate to severe RLS may experience significant sleep disruptions. Even those with milder cases of RLS may suffer from insufficient sleep.
Some of the negative effects of insufficient sleep caused by RLS include:
- Daytime sleepiness
- Diminished quality of mood
- Difficulty concentrating or thinking clearly
- Impaired performance at school or work
- Decreased productivity
- Increased irritability
- Impaired memory
- Difficulty completing daily tasks
- Reduced immune system function
- A greater risk of heart disease, stroke, diabetes, anxiety, and depression
RLS Fact: RLS is less common among African and Asian populations, suggesting that the disorder likely involves genetics, and possibly environment or diet
RLS and Sleep Partners
The symptoms of RLS may result in nightly tossing and turning, shaking or stretching the legs, and getting in and out of bed in an effort to relieve uncomfortable sensations. These movements may impact a sleeping partner, creating frequent sleep disruptions and making returning to sleep difficult.
A partner’s sleep deprivation may result in daytime fatigue, diminished cognitive abilities, reduced immune system function, and impaired work performance.
The sleep partner of a RSL sufferer may help in relieving some of the disorder’s symptoms by:
- Encouraging the person afflicted with RLS to consult a doctor. Medical treatment may help them manage the condition and its symptoms more effectively
- Massaging the affected partner’s legs or supplying them with heating pads or cold packs
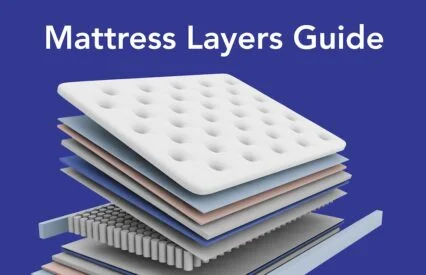
- Investing in a mattress that limits movement transfer. Separate blankets may also help
- Sleeping in a different room when the partner’s symptoms are particularly disruptive
- Adopting lifestyle changes that may benefit RLS sufferers, such as moderate exercise, healthy eating, and good sleep hygiene
Note: The content on Sleepopolis is meant to be informative in nature, but it shouldn’t taken as medical advice, and it shouldn’t take the place of medical advice and supervision from a trained professional. If you feel you may be suffering from any sleep disorder or medical condition, please see your healthcare provider immediately.
Restless Legs Syndrome Treatments
Treatment options for RLS include natural remedies, medications, and lifestyle modifications. (22) Some treatments may not eliminate RLS symptoms, but help to ease their severity and facilitate better sleep.
Mild symptoms of Restless Legs Syndrome that only minimally impact sleep may not require treatment. If RLS is linked to another medical condition, treatment may involve effective management of the original condition.
Natural Treatments and Lifestyle Modifications
Moderate RLS symptoms may be reduced by making certain lifestyle changes, such as:
- Adopting a moderate exercise program (23)
- Creating a consistent sleep schedule, and going to bed and waking up at the same time every day
- Maintaining a healthy weight (24)
- Avoiding the use of alcohol, caffeine, and nicotine
- Staying hydrated and eating a nutritious diet
- Employing relaxation techniques such as meditation, Tai Chi, acupuncture, or yoga
- Scheduling long car and/or plane rides for earlier in the day, when symptoms are less likely to be severe
- Avoiding the use of medications that may exacerbate RLS
- Utilizing treatment devices such as a foot wrap, pneumatic compression, or vibrating pad designed for RLS sufferers
Other natural treatments include massaging the legs and applying heating pads or ice packs to the affected areas of the body. Some people with RLS may be helped by calcium and magnesium supplements, which effect the contraction and relaxation of muscle fibers.
Because even low dosages of vitamins and minerals may interfere with the absorption of other elements in the body and cause toxicity, a medical professional should be consulted before beginning any treatment program.

Medications
If lifestyle changes and natural treatments are ineffective or RLS symptoms are severe, a doctor may prescribe one or more medications or minerals to treat the condition. Treatment options include:
- Dopamine-enhancing drugs such as levodopa. These drugs influence dopamine levels in the brain, and are a common treatment for conditions such as Parkinson’s Disease. While often effective, treatment of RLS with levodopa and similar drugs may lead to what’s termed “augmentation,” or a rebound effect resulting in increased symptoms (25)
- Intravenous iron supplementation. Iron treatment can be remarkably effective in RLS, with some studies showing that symptoms resolved completely in about 20% of patients (26)
- Anticonvulsants or antiseizure drugs. These may make the restlessness of RLS more bearable and help ease uncomfortable sensations in the legs
- Sleep medications and/or muscle relaxants. These may help people with RLS sleep better at night
- Drugs that influence calcium levels. While not totally clear why, these types of medications may improve RLS symptoms in some people
- Narcotic pain relievers, also known as opioids. Low doses of opioids can help relieve RLS symptoms that manifest as discomfort in the legs. The risk of tolerance to opioids in RLS sufferers may be lower than in patients with other chronic pain syndromes that require higher medication dosages (27)
A medication that alleviates symptoms in one RLS sufferer may exacerbate symptoms in another. One drug may help initially before gradually decreasing in effectiveness. There is a risk of side effects with any medication, as well as a possibility of dependence and tolerance with sleep medications, opioids, and muscle relaxants.
The Future of RSL Research
Since the diagnostic criteria for Restless Legs Syndrome was established in 1995, the disorder has been studied extensively. The exact cause of the condition remains unclear, but there is no longer debate about RSL as a real disorder.
Though RSL still has no cure, recent advances have resulted in more targeted directions for research. Some scientists theorize that iron insufficiency combined with genetics might “switch on” the disorder, which continues even after blood levels of iron return to normal. In fact, we may discover that genetics alone cause RSL in relatively few people.
Future research may target iron regulation in the brain, as well as environmental stressors that contribute to the development of RLS. This could allow researchers to prevent the development of the condition, or treat it more effectively. Whether RSL begins during pregnancy, childhood, or later in life, a better understanding of the disorder may lead to more customized and effective treatment options.
References
- MV Svetel, Quality of Life in Patients with Primary Restless Legs Syndrome: Community-based Study, National Center for Biotechnology Information, Aug. 2010
- Y. Oka, Secondary Restless Legs Syndrome, National Center for Biotechnology Information, May 2009
- M. Michaud, Arm Restlessness in Patients with Restless Legs Syndrome, Movement Disorders, Mar. 2000
- Ulrike Mitchell, Peripheral Dopamine in Restless Legs Syndrome, Frontiers in Neurology, Mar. 15, 2018
- RP Allen, The Role of Iron in Restless Legs Syndrome, Movement Disorders, June 2008
- Maurice M. Ohayon, Epidemiology of Restless Legs Syndrome: A Synthesis of the Literature, Sleep Medicine Review, Aug. 2012
- M. Michaud, Circadian Rhythm of Restless Legs Syndrome: Relationship with Biological Markers, Annals of Neurology, Mar. 2004
- Donald L. Bliwise, Medications Associated with Restless Legs Syndrome: A Case Control Study in the US Renal Data System, Sleep Medicine, Oct. 15, 2014
- A. Neyal, A Prospective Study of Willis-Ekbom Disease/Restless Legs Syndrome During and After Pregnancy, Sleep Medicine, Sep. 15, 2016
- DL Picchietti, Further Studies on Periodic Limb Movement Disorder and Restless Legs Syndrome in Children with Attention-deficit Hyperactivity Disorder, Movement Disorders, Nov. 1999
- I. Schlesinger, Restless Legs Syndrome in Stroke Patients, Sleep Medicine, Aug. 2015
- Giuseppe Plazzi, MD, Restless Legs Syndrome is Frequent in Narcolepsy with Cataplexy Patients, Sleep, May 1, 2010
- Paul Stillman, Algorithms for the Diagnosis and Treatment of Restless Legs Syndrome in Primary Care, BMC Neurology, Feb. 27, 2011
- V. Dhawan, Genetic Aspects of Restless Legs Syndrome, Postgraduate Medical Journal, Aug. 2006
- J. Winkelmann, Genetics of Restless Legs Syndrome, Current Neurology and Neuroscience Reports, May 2008
- Y. Li, Association of Multiple Sclerosis with Restless Legs Syndrome and Other Sleep Disorders in Women, Neurology, May 2012
- AJ Bentley, Gender Differences in the Presentation of Subjects with Restless Legs Syndrome, Sleep Medicine, Jan. 7, 2006
- S. Whittom, Age-at-onset in Restless Legs Syndrome: a Clinical and Polysomnographic Study, Sleep Medicine, Dec. 9, 2007
- R. Nisha Aurora, The Treatment of Restless Legs Syndrome and Periodic Limb Movement Disorder in Adults—An Update for 2012: Practice Parameters with an Evidence-Based Systematic Review and Meta-Analyses, Sleep, Aug.1, 2012
- AS Walters, Review of the Relationship of Restless Legs Syndrome and Periodic Limb Movements in Sleep to Hypertension, Heart Disease, and Stroke, Sleep, May 2009
- Richard K. Bogan, Effects of Restless Legs Syndrome on Sleep, Neuropsychiatric Disease and Treatment, Dec. 2, 2006
- Cynthia Comella, Treatment of Restless Legs Syndrome, Neurotherapeutics, Jan. 11, 2014
- Melissa McManama Aukerman, Exercise and Restless Legs Syndrome: a Randomized Controlled Trial, JABFM, Sep. 2006
- S. Lin, The Association Between Obesity and Restless Legs Syndrome: A Systemic Review and Meta-analysis of Observational Studies, Journal of Affective Disorders, Aug. 1, 2018
- RP Allen, Augmentation of the Restless Legs Syndrome with Carbidopa/Levodopa, Sleep, Apr. 1996
- Trenkwalder C, Restless Legs Syndrome Associated with Major Diseases, Neurology, Apr. 5, 2016
- Michael H. Silber, The Appropriate Use of Opioids in the Treatment of Refractory Restless Legs Syndrome, Mayo Clinic Proceedings, Nov. 2017