
Key Takeaways
- A nightmare is a bad dream that evokes strong feelings of fear, terror, or other disturbing emotions.
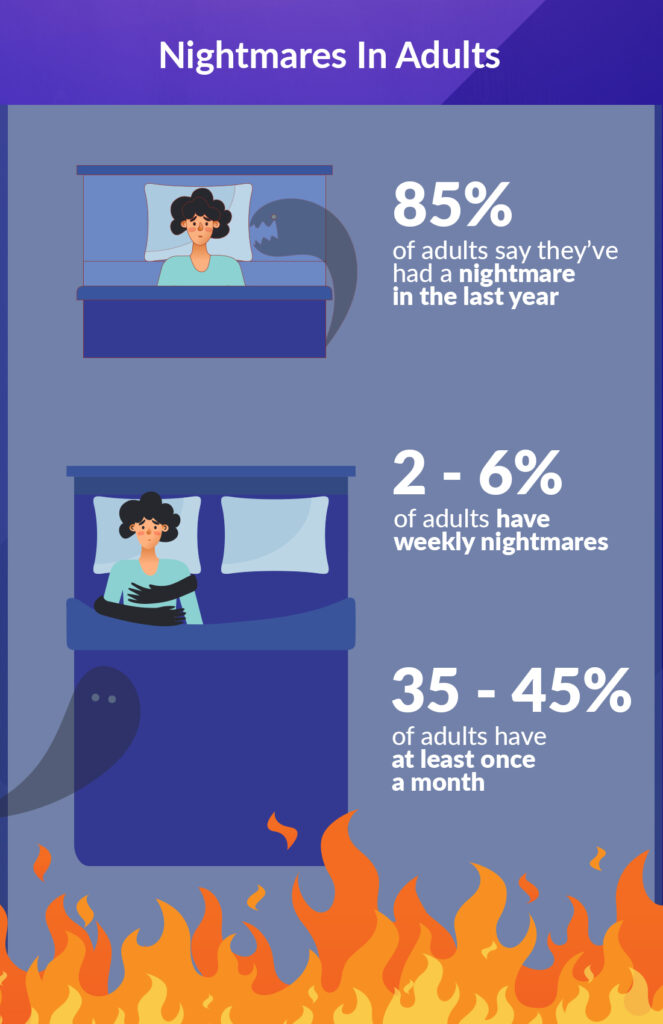
- Nightmares are relatively common, and around 85 percent of U.S. adults report having had at least one in the past year.
- Nightmares tend to occur during REM sleep and can be triggered by several things, such as stress, anxiety, or mental illness.
- Experiencing frequent nightmares that trigger distress, disrupt sleep, interfere with daytime functioning, and/or lead to fear of falling asleep may indicate a nightmare disorder.
Nightmares — vivid dreams that make you feel negative emotions — look a bit different from plain old bad dreams because they wake you up from sleep. (1) (2) Nightmares can create powerful emotions, and may trigger fear, anger, sadness, guilt, or anxiety. (3)
As rare as we might wish they were, nightmares are quite common. About 85 percent of adults have experienced a nightmare within the past year, and they’re even more prevalent in children and adolescents. (4)
Below, we’ll explain why you may have nightmares and offer some tactics to prevent these vivid dreams.
Note: The content on Sleepopolis is meant to be informative in nature, but it shouldn’t be taken as medical advice, and it shouldn’t take the place of medical advice and supervision from a trained professional. If you feel you may be suffering from any sleep disorder or medical condition, please see your healthcare provider immediately.
What Are Nightmares?
Nightmares describe disturbing, vivid dreams that cause powerful feelings of fear, distress, terror, or anxiety. (5) While everyone has a bad dream now and then, nightmares are different because they wake you from sleep. (2)
When you wake up from a nightmare, you can feel a wave of strong emotions like fear, anger, or sadness. (1) “Nightmares can be incredibly intense and distressing … leaving behind lingering feelings of fear, anxiety, or sadness,” Joel Frank, PsyD, clinical psychologist and neuropsychologist at Duality Psychological Services tells Sleepopolis. They can even cause some emotional distress during the day — long after waking. (6)
Below, we’ll help you figure out how to tell if someone is having a nightmare and what it looks like. Then, we’ll give you some options to help yourself or a loved one achieve more peaceful sleep.
How Common Are Nightmares in Adults?
A majority of people experience nightmares, no matter their age. In the general population, about 70 percent of people have them occasionally. (1)
In adults, 85 percent say they’ve had a nightmare in the last year. (4) But a much smaller group report frequent nightmares. (1) Only about two to six percent of adults have weekly nightmares, and 35 to 45 percent have them at least once a month. (3)
What Are the Most Common Nightmares?
Nightmares typically fall into two categories: physical threats and psychological threats. Physical threats can look like attacks, fighting, hurting, or killing. Psychological threats deal with your emotions and can involve themes of betrayal, rejection, embarrassment, and being abandoned. (1)
“Nightmares are deeply personal experiences shaped by the intricate tapestry of an individual’s life,” Frank tells Sleepopolis. An Amerisleep survey of 2,000 conducted in 2023 found the most common nightmares include: (7)
- Falling
- Being chased
- Dying
- Feeling lost
- Missing an important event
- Waking up late
- Paralysis
- Death of a loved one
- House fires
- Teeth falling out
It’s worth noting that since nightmares often tie to your everyday events and issues, everyone has distinctive nightmare experiences. (4) “This variation highlights the unique interplay of personal experiences, cultural influences, and individual fears that define our nocturnal visions,” says Frank.
Nightmares in Adults vs. Kids
Children and adolescents have more nightmares than adults, and up to 50 percent of kids aged three to six report them regularly. Nightmares can persist as we grow, and about 14 percent of college students still report them. But overall, nightmares happen less often as we age. (8)
Common causes of nightmares in children include: (9)
The nightmares experienced by kids and teens can have differing themes than adults. They may dream about monsters, a scary movie they watched, or separation from their parents. Older kids may start to dream about death or danger. (11)
Nightmares in kids can also begin or pick up in frequency after big or small life events, with triggers ranging from starting a new school to a parent having a cold. (5) “Children might seek comfort from parents after nightmares, while adults may carry anxiety throughout the day, influenced by their coping strategies and maturity,” says Frank.
No matter your age, nightmares aren’t much fun. Let’s look at why nightmares happen and then talk about possible solutions.
Why Do We Have Nightmares?
Experts aren’t positive why we have nightmares, but these vivid dreams may come from a tiny spot in your brain: the amygdala. This small structure helps you deal with threats — an important job!
Still, some experts have theories. When you get deep into rapid-eye movement (REM) sleep, your dreams get extra vivid. When this happens, your amygdala may think you’re under attack and try to create mental scenarios to prepare you for danger. (4) (6) Now, that’s just a theory, and some experts don’t think the amygdala causes nightmares — only responds to them. (6)
Other parts of the brain get active during nightmares, but researchers have yet to pinpoint the exact mechanism behind them. (6) Some say nightmares don’t serve a purpose, but others say they can help you regulate your emotions. (3) Either way, we need a lot more information to fully understand the “why” behind nightmares.
Signs and Symptoms of Nightmares in Adults
Symptoms of nightmares are usually obvious because of the strong emotions that come with these dreams and the likelihood that you’ll remember them.
Typical signs and symptoms may include: (1) (12)
- Experiencing dreams with disturbing or upsetting themes, such as death, threat to physical safety, war, or personal conflict
- Sitting upright in bed after a dream
- Waking feeling anxious
- Waking with an increased breathing or heart rate
- Crying after a dream
- Waking up sweaty
- Waking from sleep screaming or shouting
- A strong feeling of fear after waking
Nightmares may make returning to sleep difficult, especially if they cause physical symptoms like increased heart rate, sweating, or feeling shaky. (1) (13) You may wish you could avoid these symptoms, but to know how to do that, you need to understand what causes these intense dreams.
What Causes Nightmares?
Ordinary nightmares may be triggered by simple causes, but they can also come from more complex experiences or medical conditions. Occasionally, eating before bed or watching a scary show can prompt a nightmare while you sleep. (5)
However, nightmares can also be caused by bigger issues, including:
- Stress and anxiety: Major life changes or everyday conflicts with friends can prompt stress and anxiety, which can boost your risk of nightmares. (5) (12)
- Post-traumatic stress disorder (PTSD): Accidents, abuse, injury, or any traumatic event can cause nightmares, which are especially common in people with PTSD. When you have PTSD, you can have nightmares each time you fall asleep. This can make you avoid bedtime, leading to sleep deprivation. (14)
- Fever: The extra heat from a fever can lead to more bizarre and negative dreams. (10)
- Sleep deprivation: When you don’t get enough good-quality sleep, your brain will push you into more REM sleep to prioritize that sleep stage (called REM rebound). Longer periods of REM sleep can lead to more nightmares. (2)
- Insomnia: Insomnia, a sleep disorder causing issues falling and staying asleep, can also trigger longer REM periods. And more REM equals higher risk for nightmares. (8) (15)
- Substance use: Taking in too much alcohol or recreational drugs can trigger nightmares. Withdrawal from these substances can do the same. (12)
- Depression: Nightmares are more common in people with depression. (16) But it goes both ways. For example, if you have nightmares and insomnia, you could have a higher risk of depression. (17)
- Pregnancy: When you’re pregnant, hormone changes can prompt nightmares. (18) Also, pregnancy discomfort can steal your sleep, leading to REM rebound, which can lengthen your REM sleep and cause more nightmares. (8)
- Medications: Some medications like benzodiazepines (like alprazolam) or barbiturates (like phenobarbital) can cause withdrawal when you stop them. Stopping these drugs can cause REM sleep rebound and nightmares. (5) Other medications for depression, heart disease, Parkinson’s disease, and a range of other disorders can also increase your risk for nightmares. (3) (12) (19)
Now that you have the full list of nightmare-causing culprits, we can talk about what nightmares do to your sleep.
How Can Nightmares Affect Sleep?
Nightmares are defined by abrupt awakening from sleep. Sleep interruptions of any kind aren’t great, but after jolting awake from a terrifying dream, you may find it hard to drift off again. (20)
These wake-ups mean disrupted snoozing and sleep deprivation, which can make you feel tired the next day. It can even affect how you work, learn, focus, and function while awake. You may also feel more cranky and have trouble judging situations and reacting appropriately. (21)
Beyond crankiness, people who have nightmares report more anxiety, sadness, and distress during the day, as well as more physical pain and less overall well-being. (22) Regular nightmares can lower your quality of life and are even associated with higher rates of suicide. (3)
If you have thoughts of harming yourself, call or text 988 for immediate help. (23)
When you think you’ll have a nightmare as you snooze, you may avoid bedtime for as long as you can. But going to bed later can lead to less overall sleep, and sleep deprivation can worsen nightmares. (3) (4)
This may feel like tough stuff. But hang in there — we need to talk about nightmare disorders and then we’ll give you some options for more peaceful sleep.
What Is Nightmare Disorder?
Nightmare disorder causes frequent terrifying nightmares that wake you up repeatedly and can’t be explained by other mental health disorders. (4)
Nightmares are common experiences that can affect anyone, says Frank. “However, when these nightmares become frequent and intense enough to significantly impact daily life, they may be classified as a nightmare disorder.”
This disorder can range in severity based on the average occurrence of nightmares: (24)
- Mild: Fewer than one nightmare per week
- Moderate: One or more nightmares per week (but not every night)
- Severe: At least one nightmare every night
Regardless of severity, nightmare disorders can be called acute or chronic. Acute means they last one month or less. Chronic nightmare disorder lasts for at least six months, and “subacute” nightmare disorder takes up the space in between. (24)
About two to eight percent of Americans have a nightmare disorder. (24) The dreams of nightmare disorder are different from ordinary nightmares — they’re longer, more vivid, and affect your daytime functioning. Nightmare disorder may also lead to insomnia because of chronic anxiety and the fear of falling asleep. (12)
Yikes, that’s intense! But now that you know all about nightmares, you can read how to trade in those disturbing dreams for better sleep.
Treatment for Nightmare Disorder
You may need treatment for nightmare disorder if your dreams cause extra distress, disturb your sleep, and interfere with day-to-day activities. (12) The cause of the nightmare disorder helps determine treatment.
Nightmare disorder treatment options may include: (25)
- Stress-reduction techniques: Mindfulness, meditation, deep breathing, and yoga can all decrease overall stress, which may lessen your nightmares. (26)
- Counseling: Speaking with a mental health professional may help you get to the root of your nightmare triggers and address them.
- Imagery rehearsal therapy: Most often used with people who have nightmares with PTSD, imagery rehearsal therapy can help you adjust the content of your nightmares by imagining more happy endings. (27)
- Medical treatment: If your nightmares stem from a medical condition, treating that condition can lessen nightmares.
- Medications: Although rarely used, some medications may help with nightmares, especially for severe nightmares with PTSD. (28)
Nightmares vs. Night Terrors
Unlike nightmares, night terrors (a type of sleep disorder called parasomnia) usually happen during non-REM sleep and include more outward symptoms like yelling, screaming, and thrashing in bed. (29)
How to Prevent Nightmares in Adults
When it comes to preventing nightmares, you can use several techniques, some of which may overlap with treatment options. For example, relaxation techniques can melt away stress and prepare you for a nightmare-free snooze fest. (30)
Not only do yoga, meditation, and guided relaxation therapies help lower stress and anxiety, they may lessen your fear of nightmares and sleep avoidance. “Preventing nightmares can involve adopting lifestyle changes and implementing psychological strategies aimed at promoting peaceful sleep,” says Frank.
A relaxing bedtime routine may also help reduce anxiety and help reduce the risk of disturbing dreams. (25) In addition to relaxing routines, good sleep hygiene practices can also help you sleep better and fend off nightmares. (3)
Good sleep hygiene includes: (25) (31)
- Keeping a consistent sleep schedule
- Making your bedroom calm, quiet, dark, and comfortable
- Avoiding screens before bed
- Steering clear of alcohol, caffeine, and nicotine too close to bedtime
- Sticking to light snacks before sleep
Using these tips, you can set yourself up for sleep success and hopefully skip any nightmares that may try to steal your rest.
When to See a Doctor
If your nightmares are interfering with your sleep and daily life, it may be time to speak to a healthcare provider. Frank suggests speaking to a provider if you experience:
- Frequent distressing nightmares
- Impairment in daily life
- Chronic sleep deprivation
- Increased anxiety
- Resistance to lifestyle changes aimed at reducing nightmares
Also be sure to ask for medical help if your nightmares began or worsened after you started a new medicine, or if they happen after heavy use of alcohol or drugs and you don’t feel you can cut back on your own. (5)
A provider can help you get to the bottom of your nightmare triggers and make a plan to shoo them away. They may also recommend speaking with a sleep therapist or another mental health professional.
FAQs
Why do I keep having nightmares?
You may have regular nightmares for several reasons, including mental health conditions like depression and PTSD, medical issues like pregnancy, sleep disorders like insomnia, and even some medications.
How can I stop having nightmares every night?
You can try to prevent nightmares with de-stressing activities like yoga, meditation, mindfulness, and deep breathing. If your nightmares are persistent, you can ask a healthcare provider about further treatment like counseling and medical treatment.
Why does melatonin give me nightmares?
Melatonin may give you nightmares because it can increase the time you spend in REM sleep. You have your most vivid dreams in this sleep stage, so it may leave with you with more to have and remember nightmares. (32)
Are vivid dreams a sign of mental illness?
No, vivid dreams don’t mean you have a mental illness. But nightmares can be more common in people with mental illnesses like depression and PTSD.
The Last Word From Sleepopolis
Nightmares are extremely frightening dreams that wake you up from sleep. Whether from stress, anxiety, sleep disorders,or pregnancy, they can wake you up feeling like you narrowly escaped a massive threat.
If you’d like to squash those nightmares, it’s important to treating any condition that triggers them. You can also talk it over with a mental health professional, and adopt some stress-relieving activities through the day (and good sleep habits before bed).
If your nightmares affect your everyday life, you can ask a healthcare provider for help. They can help you keep those nightmares at bay!
Sources
- Faccini J, Del-Monte J. Bad dream, nightmares and psychopathology: a systematic review. Front Psychiatry. 2024;15:1461495. doi:10.3389/fpsyt.2024.1461495
- Nightmares in adults: Symptoms, causes, and innovative, science-backed therapies. Accessed November 13, 2024. https://www.apa.org/monitor/2024/10/science-of-nightmares
- Skeie-Larsen M, Stave R, Grønli J, et al. The Effects of Pharmacological Treatment of Nightmares: A Systematic Literature Review and Meta-Analysis of Placebo-Controlled, Randomized Clinical Trials. International Journal of Environmental Research and Public Health. 2023;20(1):777. doi:10.3390/ijerph20010777
- McNamara P, Wildman WJ, Hodulik G, Rohr D. A neurocomputational theory of nightmares: the role of formal properties of nightmare images. Sleep Adv. 2021;2(1):zpab009. doi:10.1093/sleepadvances/zpab009
- Nightmares: MedlinePlus Medical Encyclopedia. Accessed November 13, 2024. https://medlineplus.gov/ency/article/003209.htm
- Nadorff MR, Titus CE, Pate AR. A Meaningful Step Toward Understanding the Cause and Impact of Nightmares. J Clin Sleep Med. 2019;15(2):179-180. doi:10.5664/jcsm.7608
- The most common nightmares — and how to cope with them. Accessed November 13, 2024. https://nypost.com/2024/10/29/lifestyle/the-most-common-nightmares-and-how-to-cope-with-them/
- REM Rebound Effect – StatPearls – NCBI Bookshelf. Accessed November 13, 2024. https://www.ncbi.nlm.nih.gov/books/NBK560713/
- When Do Kids Start Having Nightmares? Accessed November 13, 2024. https://health.clevelandclinic.org/nightmares-in-children
- Schredl M, Erlacher D. Fever Dreams: An Online Study. Front Psychol. 2020;11:53. doi:10.3389/fpsyg.2020.00053
- Nightmares In Children | Children’s Hospital Colorado. Accessed November 13, 2024. https://www.childrenscolorado.org/conditions-and-advice/conditions-and-symptoms/conditions/nightmares/
- Nightmare disorder – Symptoms and causes – Mayo Clinic. Accessed November 13, 2024. https://www.mayoclinic.org/diseases-conditions/nightmare-disorder/symptoms-causes/syc-20353515
- Hess G, Schredl M, Gierens A, Domes G. Effects of nightmares on the cortisol awakening response: An ambulatory assessment pilot study. Psychoneuroendocrinology. 2020;122:104900. doi:10.1016/j.psyneuen.2020.104900
- Lancel M, van Marle HJF, Van Veen MM, van Schagen AM. Disturbed Sleep in PTSD: Thinking Beyond Nightmares. Front Psychiatry. 2021;12. doi:10.3389/fpsyt.2021.767760
- Reffi AN, Moore DA, Drake CL. Objective sleep disturbance in nightmares: is prolonged sleep onset latency a proxy for fear-of-sleep-related arousal? Sleep. 2024;47(4):zsae040. doi:10.1093/sleep/zsae040
- Depression and insomnia are linked to frequent nightmares. Accessed November 13, 2024. https://sleepeducation.org/depression-insomnia-linked-frequent-nightmares/
- Ollila HM, Sinnott-Armstrong N, Kantojärvi K, et al. Nightmares share genetic risk factors with sleep and psychiatric traits. Transl Psychiatry. 2024;14(1):1-6. doi:10.1038/s41398-023-02637-6
- Bušková J, Miletínová E, Králová R, et al. Parasomnias in Pregnancy. Brain Sci. 2023;13(2):357. doi:10.3390/brainsci13020357
- Gill P, Fraser E, Tran TTD, et al. Psychosocial treatments for nightmares in adults and children: a systematic review. BMC Psychiatry. 2023;23(1):283. doi:10.1186/s12888-023-04703-1
- Nightmares – Sleep Education by American Academy of Sleep Medicine. Accessed November 13, 2024. https://sleepeducation.org/sleep-disorders/nightmares/
- Sleep Deprivation and Deficiency – What Are Sleep Deprivation and Deficiency? | NHLBI, NIH. Accessed November 4, 2023. https://www.nhlbi.nih.gov/health/sleep-deprivation
- Mallett R, Picard-Deland C, Pigeon W, et al. The Relationship Between Dreams and Subsequent Morning Mood Using Self-Reports and Text Analysis. Affect Sci. 2022;3(2):400-405. doi:10.1007/s42761-021-00080-8
- 988 Lifeline – If you need emotional support, reach out to the national mental health hotline: 988. Accessed November 13, 2024. https://988lifeline.org/
- Nightmare Disorder: What It Is, Symptoms & Treatment. Accessed November 13, 2024. https://my.clevelandclinic.org/health/diseases/24464-nightmare-disorder
- Nightmare disorder – Diagnosis and treatment – Mayo Clinic. Accessed November 13, 2024. https://www.mayoclinic.org/diseases-conditions/nightmare-disorder/diagnosis-treatment/drc-20353520
- Mindfulness exercises – Mayo Clinic. Accessed May 10, 2024. https://www.mayoclinic.org/healthy-lifestyle/consumer-health/in-depth/mindfulness-exercises/art-20046356
- Romier A, Clerici E, Stern E, Maruani J, Geoffroy PA. Therapeutic Management of Nightmares: Practice Guide for Imagery Rehearsal Therapy (IRT). Curr Sleep Medicine Rep. 2024;10(2):139-154. doi:10.1007/s40675-024-00287-8
- Sheaves B, Rek S, Freeman D. Nightmares and psychiatric symptoms: A systematic review of longitudinal, experimental, and clinical trial studies. Clin Psychol Rev. 2023;100:102241. doi:10.1016/j.cpr.2022.102241
- Van Horn NL, Street M. Night Terrors. In: StatPearls. StatPearls Publishing; 2023. Accessed September 15, 2023. http://www.ncbi.nlm.nih.gov/books/NBK493222/
- Aetiology and treatment of nightmare disorder: State of the art and future perspectives – Gieselmann – 2019 – Journal of Sleep Research – Wiley Online Library. Accessed November 13, 2024. https://onlinelibrary.wiley.com/doi/10.1111/jsr.12820
- Baranwal N, Yu PK, Siegel NS. Sleep physiology, pathophysiology, and sleep hygiene. Progress in Cardiovascular Diseases. 2023;77:59-69. doi:10.1016/j.pcad.2023.02.005
- Can Melatonin Cause Bad Dreams? What Experts Say. Accessed November 13, 2024. https://health.clevelandclinic.org/does-melatonin-cause-bad-dreams
Joel Frank. Personal Interview. November 12, 2024.



























