Getting enough high-quality rest can be a challenge for anyone, but when you have attention-deficit/hyperactivity disorder (ADHD), good sleep is even more elusive. ADHD can cause you to daydream through the workday, lose your keys (a lot), fidget, and talk a mile a minute. Then, when evening arrives, you might face challenges in winding down due to impulsivity and self-regulation issues, which can make it hard to transition to more restful activities like sleep. (1)
Different types of ADHD can cause different sleep issues, and the best treatment options vary from person to person. But you can get better sleep even if you have ADHD, and we can help you figure out where to start.
Long Story Short
- ADHD and sleep problems can feed off each other and cause similar symptoms like memory issues and daytime sleepiness.
- Sleep disorders are also common in those with ADHD, showing up in 60 to 80 percent of people with the disorder.
- It may be harder to get good sleep with ADHD because of unpredictable sleep schedules, stimulant medications, and coexisting mental health disorders.
- If you have ADHD, you can improve your sleep by following good sleep hygiene practices and trying different tricks like snuggling under a weighted blanket. If these don’t help, your healthcare provider can work with you to find the right treatment for better rest.
The Relationship Between ADHD and Sleep
ADHD and sleep have a complex relationship, Dr. Chester Wu, MD, sleep medicine physician in Houston, TX, tells Sleepopolis. “ADHD can lead to difficulties in falling and staying asleep due to overactivity of the brain, and inadequate sleep can exacerbate ADHD symptoms (such as impulsivity, lack of focus, hyperactivity, and behavioral issues), creating a cycle of restlessness and inattention,” Wu says.
Research tells us that sleep and circadian rhythm disturbances may contribute to ADHD development, he adds. And sleep deprivation can also mimic ADHD symptoms, which can make it hard for healthcare providers to make the right diagnosis. All this contributes to significant crossover between the two—sleep disorders show up in 60 to 80 percent of people with ADHD. (2) (3)
ADHD, Sleep, and the Brain
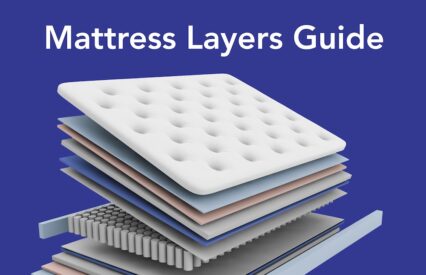
If you have ADHD, your brain works a little bit differently. The nerve networks in your brain serve as a busy set of highways and back roads for neurotransmitters (brain messengers) to zip along. In a brain with ADHD, these highways are built in unique patterns and some neurotransmitters are more sparse. (4) Completing a successful night’s sleep requires a lot of communication in the brain, and if certain messengers are in short supply, sleep can be delayed or interrupted. (5) (6)
ADHD Meds Can Keep You Up
A group of medications termed “stimulants” are a common treatment type for ADHD. But as the name implies, they aren’t great for sleep. Stimulants help the brain focus but can keep you buzzing well into the night. (3) Read on to find out some tips and tricks to counteract these effects.
Mental Health, ADHD, and Sleep
Mental health and sleep are closely intertwined. Because ADHD affects your sleep, it can also put you at a higher risk for some mental health disorders, like: (2) (7)
- Anxiety disorders
- Bipolar disorder
- Depression
When you have other mental health symptoms, they can sometimes mask your ADHD symptoms. (2) While ADHD and mental health issues don’t do much to help you get solid sleep, the good news is that when you treat one, the others can fall in line more easily, like a positive domino effect.
ADHD, Sleep, and Daily Life
When ADHD steals your sleep, it can have a big impact on daily life. “I often say that when it comes to sleep, we are no different than toddlers,” says Bassi. “A lack of sleep makes us cranky and impulsive.” Sleep deprivation can also cause: (12)
- Excessive daytime sleepiness
- Fatigue
- Moodiness
- Trouble concentrating
- Decreased libido
If you have ADHD and aren’t getting enough zzzs, that sleep loss can make your ADHD symptoms harder to manage. (10) Sleep deprivation messes with the part of your brain that helps you pay attention and remember the things you need to, says Bassi. “Therefore, it makes all the ADHD symptoms appear worse.” (7)
Bassi adds that sometimes patients come to the office concerned about their ADHD symptoms, but it turns out that a sleep issue is the culprit. When they treat the sleep problem, the ADHD symptoms ease up.
Common Sleep Challenges for People with ADHD
ADHD doesn’t look the same for everyone: people with the inattentive type might have trouble paying attention when they need to, while those with hyperactive or impulsive ADHD might fidget constantly or make rash decisions. (8) But all ADHD types can cause a host of challenges with regard to sleep.
Procrastination Causing Late Nights
Inattentive ADHD can make it hard to manage your time well, leading to procrastination and later bedtimes. “Often, [people with ADHD] will feel a sense of pressure to get work accomplished at night because the clock is ticking down and they have no more opportunity to procrastinate,” says Dr. Bruce Bassi, MD, a psychiatrist based in Chicago. This can lead to those with ADHD starting new projects right as they should be winding down for sleep, he says.
Too Much Excitement
When your brain is vibrating with good ideas and excitement, it’s hard to convince yourself it’s time to drift off. Pretty much everyone can relate to the occasional hamster wheel in your head going at a furious pace when you just want to sleep, but those with ADHD are accustomed to dealing with that experience night after night. (3)
Chaotic Sleep Schedule
Have you ever gotten going on a fun project late at night, and find you’ve stayed up into the wee hours? If you have ADHD, this scenario might be more the norm than the exception. Late nights can be fun, but regular bedtimes are a huge part of getting good, consistent sleep.
When your sleeping schedule is all over the place, it can also confuse your internal clock (circadian rhythm), so that your brain doesn’t realize it’s time to wind down. Many adolescents with ADHD report staying up all night and falling asleep in class. (3) One study found adults with ADHD went to bed 39 minutes later than those without the disorder, were more likely to take an hour to fall asleep on average each night, and were more to report daytime sleepiness than those without ADHD. (9)
Common Sleep Disorders for People with ADHD
Some sleep issues in ADHD can stem from bad bedtime habits, but sometimes problems with snoozing can come from a sleep disorder.
Insomnia
If you have insomnia, it can be hard to fall asleep, stay asleep, or get high-quality slumber in general. (11) People with ADHD complain of insomnia more than any other sleep disorder. Experts think insomnia with ADHD can stem from other sleep disorders, poor sleep hygiene, and stimulant medications. (3)
Excessive Daytime Sleepiness
Anyone can feel sleepy after a rough night, but excessive daytime sleepiness is, well, excessive. Excessive daytime sleepiness, or EDS, describes more than just a slow morning—it can cause problems in work or school tasks and can even up the risk of driving accidents. (12) Up to 40 percent of people with ADHD have EDS, and it can be caused by habitually bad sleep or sleep disorders. (2)
Restless Leg Syndrome
People with restless leg syndrome (RLS) describe an uncomfortable and unpleasant sensation in their legs that grows until they feel an uncontrollable urge to move them. (13) It’s hard to fall asleep when your legs are forced to do the occasional dance move in bed, and RLS can cause difficulty staying asleep, too. Unfortunately, ADHD and RLS often come as a package deal. (14) More research is needed to understand the link between RLS and ADHD, but the existing findings may point to a potential common physiological pathway, such as sleep fragmentation.
Narcolepsy
Ever feel like dropping off to sleep at your desk? On a Zoom call? While listening to your spouse? (We won’t tell) Well, if you have narcolepsy, you can fall asleep anytime, anywhere, and mostly without warning. (15)
New research is looking at the connection between narcolepsy and ADHD. (2) While experts don’t know for sure how they are connected, one possible link is disrupted sleep, which plays a major role in both conditions. (16)
Circadian Rhythm Disorders
Circadian rhythm disorders (CRDs) get your internal clock all out of whack and disrupt your sleep patterns. (17) The diverse bedtimes that those with ADHD lean toward can quickly confuse their internal clock. About 73 to 78 percent of people with ADHD report a circadian rhythm disorder, making it one of the most common of the bunch. (18)
Sleep Apnea
When you have sleep apnea, your breaths get interrupted throughout the night, either by a physical blockage in your throat (tongue or tonsils) or by confused signals from your brain. (19) Recent studies have found that ADHD and sleep apnea may be connected in children, but more research is needed to understand why. (20) (21)
ADHD and Children
ADHD isn’t just a disorder adults have — according to the Centers for Disease Control and Prevention (CDC), “the estimated number of children aged 3–17 years ever diagnosed with ADHD, according to a national survey of parents, is 6 million (9.8%) using data from 2016-2019.” (22) And as is the case with many things, kids and adults can experience ADHD differently, especially when it comes to sleep. (23) “Children with ADHD often experience more pronounced sleep issues, such as nightmares and sleepwalking, and they may struggle with excessive daytime sleepiness, impacting their academic and behavioral performance in school,” Wu says.
On the other hand, Wu adds, adults can deal more easily with circadian rhythm challenges and may not feel as sleepy as children do during the day. Children with ADHD get a lot less sleep than their peers without the disorder, and show behaviors like: (24)
- Fighting parents on bedtimes
- Taking a long time to fall asleep
- Waking up throughout the night and early in the morning
Children with ADHD are more likely to skimp on physical activity and spend too much time on screens, both of which can have a negative impact on sleep. (25) Kids are less able to self-reflect on their sleep quality and make decisions that allow for better snooze time, says Bassi. “Also, adults might be better able to communicate that they are concerned about their sleep than children… because adults have more experience to compare how their sleep is to their past.”
Sleep Tips for Children and Adults with ADHD
While children and adults with ADHD may have some different sleep symptoms, each group can improve their sleep with the same techniques. For example, anyone with ADHD can work on going to bed at the same time each night.
“Sleeping at regular intervals is critically important, therefore I would recommend that all ADHD patients set an alarm for bedtime, too. The alarm would remind you to start your bedtime routine and not start any new projects,” Bassi says. Here are some other tips you can try:
- Avoid caffeine and alcohol before bedtime
- Fit in some exercise during the day
- Keep your bedroom dark, cool, and quiet
- Avoid blue light before bed and make your sleeping space a screen-free zone
- Stick with light snacks before bed – no big meals
- Try using a weighted blanket
- Choose activities that quiet your mind come bedtime and prioritize a relaxing bedtime routine
The more you can make a sleeping area a sleep oasis, the more you or your child will want to be there. These tips aren’t the whole picture – you can try different options that sound good to you. “Over time,” says Bassi, “you’ll notice that you are falling asleep more quickly and waking up feeling more rested.”
Common Medical Treatments for Sleep Challenges with ADHD
When sleep tips and tricks don’t cut it, you might be ready for medical treatments. Whether through medications or various therapies, your healthcare provider can help you figure out which to try first.
Medication
Getting better sleep doesn’t always require adding a pill or two—sometimes the meds you’re taking now just need a little tweaking. “Medication adjustments can… play a crucial role as some ADHD medications (particularly stimulant medications) can interfere with sleep,” Wu says.
As we covered above, common ADHD medications like Concerta can do wonders for your ADHD symptoms but then keep you up when you’re ready to rest. Research suggests taking your long-acting stimulant earlier in the day can help allay problems falling asleep. (3)3 (26)26
Therapies
The first thing your provider may want you to try is behavioral treatment, which is the top remedy for insomnia across the board. (3)(11) “Behavioral interventions, such as relaxation techniques and cognitive-behavioral therapy (CBT), can be beneficial to address anxiety or other emotional issues that might be disrupting sleep,” says Wu.
One study found that children who used behavioral therapies just two or three times reported better quality of life and daytime functioning. (Parent anxiety also improved.) (24) “Behavioral therapy” can sound generic and confusing, but it can be as simple as deep breathing exercises right before sleep to calm your heart rate and quiet your mind.
Cognitive behavioral therapy for insomnia (CBT-I), on the other hand, is administered by a licensed professional who helps you pinpoint the behaviors, thoughts, and anxieties that are disrupting your sleep. Once you know this, your therapist can help you come up with techniques to restructure your thoughts and feelings and bring on the slumber. (27)
Another simple treatment option is light therapy, which helps sort out circadian rhythm problems and resets your biological clock, says Wu. Light therapy involves sitting in front of a light source at certain times of day to help your brain reset its circadian rhythm. (11)
It’s also important to take a look at any underlying conditions that can affect your sleep. “In some cases, addressing co-occurring conditions like depression or anxiety, possibly with medication or therapy, is crucial,” says Wu.
The Last Word From Sleepopolis
When ADHD interferes with restful sleep, it can cause all the normal symptoms of missing zzzs, plus compounded ADHD symptoms. Ultimately, the two together can have a snowball effect. But if you can improve the quality and quantity of your sleep other issues often fall in line. If you’ve tried all the tips you can get your hands on and you still can’t sleep, it might be time to loop in your healthcare provider. Your provider can help you address the cyclical symptoms of poor sleep and ADHD and start you on the path to better outcomes for both.
Sources
- What is ADHD? | CDC. Accessed September 30, 2024. https://www.cdc.gov/ncbddd/adhd/facts.html#SignsSymptoms
- Weibel S, Menard O, Ionita A, et al. Practical considerations for the evaluation and management of Attention Deficit Hyperactivity Disorder (ADHD) in adults. L’Encéphale. 2020;46(1):30-40. doi:10.1016/j.encep.2019.06.005
- Becker SP. ADHD and sleep: recent advances and future directions. Current Opinion in Psychology. 2020;34:50-56. doi:10.1016/j.copsyc.2019.09.006
- ADHD & the Brain. Accessed October 3, 2024. https://www.aacap.org/AACAP/Families_and_Youth/Facts_for_Families/FFF-Guide/ADHD_and_the_Brain-121.aspx
- Shen C, Luo Q, Chamberlain SR, et al. What Is the Link Between Attention-Deficit/Hyperactivity Disorder and Sleep Disturbance? A Multimodal Examination of Longitudinal Relationships and Brain Structure Using Large-Scale Population-Based Cohorts. Biological Psychiatry. 2020;88(6):459-469. doi:10.1016/j.biopsych.2020.03.010
- Brain Basics: Understanding Sleep | National Institute of Neurological Disorders and Stroke. Accessed October 3, 2024. https://www.ninds.nih.gov/health-information/public-education/brain-basics/brain-basics-understanding-sleep
- Scott AJ, Webb TL, Martyn-St James M, Rowse G, Weich S. Improving sleep quality leads to better mental health: A meta-analysis of randomised controlled trials. Sleep Medicine Reviews. 2021;60:101556. doi:10.1016/j.smrv.2021.101556
- NIMH » Attention-Deficit/Hyperactivity Disorder in Adults: What You Need to Know. Accessed October 3, 2024. https://www.nimh.nih.gov/health/publications/adhd-what-you-need-to-know
- Surman CBH, Walsh DM. Managing Sleep in Adults with ADHD: From Science to Pragmatic Approaches. Brain Sciences. 2021;11(10):1361. doi:10.3390/brainsci11101361
- Sleep Deprivation – StatPearls – NCBI Bookshelf. Accessed October 3, 2024. https://www.ncbi.nlm.nih.gov/books/NBK547676/
- Insomnia – Causes and Risk Factors | NHLBI, NIH. Accessed September 14, 2024. https://www.nhlbi.nih.gov/health/insomnia/causes
- Gandhi KD, Mansukhani MP, Silber MH, Kolla BP. Excessive Daytime Sleepiness. Mayo Clinic Proceedings. 2021;96(5):1288-1301. doi:10.1016/j.mayocp.2020.08.033
- Restless Legs Syndrome | National Institute of Neurological Disorders and Stroke. Accessed September 14, 2024. https://www.ninds.nih.gov/health-information/disorders/restless-legs-syndrome
- Migueis DP, Lopes MC, Casella E, Soares PV, Soster L, Spruyt K. Attention deficit hyperactivity disorder and restless leg syndrome across the lifespan: A systematic review and meta-analysis. Sleep Medicine Reviews. 2024;69:101770. doi:10.1016/j.smrv.2023.101770
- Narcolepsy – Narcolepsy | NHLBI, NIH. Accessed September 14, 2024. https://www.nhlbi.nih.gov/health/narcolepsy#
- Kim J, Lee GH, Sung SM, Jung DS, Pak K. Prevalence of attention deficit hyperactivity disorder symptoms in narcolepsy: a systematic review. Sleep Medicine. 2020;65:84-88. doi:10.1016/j.sleep.2019.07.022
- Circadian Rhythm Disorders – Types | NHLBI, NIH. Accessed September 16, 2024. https://www.nhlbi.nih.gov/health/circadian-rhythm-disorders/types
- Bijlenga D, Vollebregt MA, Kooij JJS, Arns M. The role of the circadian system in the etiology and pathophysiology of ADHD: time to redefine ADHD? ADHD Atten Def Hyp Disord. 2019;11(1):5-19. doi:10.1007/s12402-018-0271-z
- Sleep Apnea – Causes and Risk Factors | NHLBI, NIH. Accessed September 14, 2024. https://www.nhlbi.nih.gov/health/sleep-apnea/causes
- Hesselbacher S, Aiyer AA, Surani SR, Suleman AA, Varon J. A Study to Assess the Relationship between Attention Deficit Hyperactivity Disorder and Obstructive Sleep Apnea in Adults. Cureus. Published online October 24, 2019. doi:10.7759/cureus.5979
- Prajsuchanai T, Tanphaichitr A, Hosiri T, et al. Prevalence of high-risk for obstructive sleep apnea in attention deficit hyperactivity disorder children referred to psychiatry clinic and impact on quality of life. Front Psychiatry. 2022;13:926153. doi:10.3389/fpsyt.2022.926153
- Data and Statistics About ADHD | CDC. Accessed November 2, 2024. https://www.cdc.gov/ncbddd/adhd/data.html
- Wajszilber D, Santisteban JA, Gruber R. Sleep disorders in patients with ADHD: impact and management challenges. NSS. 2018;Volume 10:453-480. doi:10.2147/NSS.S163074
- Becker SP. ADHD and sleep: recent advances and future directions. Current Opinion in Psychology. 2020;34:50-56. doi:10.1016/j.copsyc.2019.09.006
- Tandon PS, Sasser T, Gonzalez ES, Whitlock KB, Christakis DA, Stein MA. Physical Activity, Screen Time, and Sleep in Children With ADHD. Journal of Physical Activity and Health. 2019;16(6):416-422. doi:10.1123/jpah.2018-0215
- Faraone SV, Po MD, Komolova M, Cortese S. Sleep-Associated Adverse Events During Methylphenidate Treatment of Attention-Deficit/Hyperactivity Disorder: A Meta-Analysis. J Clin Psychiatry. 2019;80(3). doi:10.4088/JCP.18r12210
- Rossman J. Cognitive-Behavioral Therapy for Insomnia: An Effective and Underutilized Treatment for Insomnia. American Journal of Lifestyle Medicine. 2019;13(6):544-547. doi:10.1177/1559827619867677
- Wu, Chester, MD. Personal Interview. October 3, 2024.