Key Takeaways
- Sleep is essential for overall health and well-being, supporting brain function as well as physical, mental, and emotional health throughout your life.
- Most adults need at least seven or more hours of sleep each night. (1)
- Nearly 20 percent of American adults get less than five hours of sleep a night (2) (3)
- It is estimated that one-third of our lives are spent sleeping. (4)
- Once thought to be purely passive, extensive research has found that sleep is an active period of recovery and preparation for the challenges of the day ahead. (5)
With all that we know about sleep, the thing that we spend a third of our lives doing remains shrouded in mystery. And while questions like ‘Why do we need sleep?’ persist, sleep science has helped us understand the importance of sleep and the goings-on under cover of night. Dylan Petkus, M.D., tells Sleepopolis that “Sleep is essential because it’s the body’s way of hitting the reset button. He explains that when we sleep, our brain sorts through memories, our body repairs cells and tissues, and hormones that regulate everything from growth to stress are balanced.” (6, 7, 8)
Petkus compares sleep to charging the battery on your phone. He says, “Without enough sleep, you’re running on low battery, which affects everything from how well you think to how strong your immune system is.” Here’s more on the benefits of sleep.
Note: The content on Sleepopolis is meant to be informative in nature, but it shouldn’t be taken as medical advice, and it shouldn’t take the place of medical advice and supervision from a trained professional. If you feel you may be suffering from any sleep disorder or medical condition, please see your healthcare provider immediately.
Why Is Sleep Important?
The benefits of sleep extend into our overall health and wellness. Physically, sleep plays a key role in our body’s growth and repair processes. Emotionally and mentally, sleep regulates our emotions and keeps our cognitive function sharp. (9) (10)
Immune System Function
Sleep keeps you healthy and fights disease by releasing cytokines (proteins that control inflammation and infection) and funneling T cells toward lymph nodes to bolster your body’s immune system’s response. (11, 12, 13)
“Think of sleep as the time when our immune system’s army — called cytokines — gets restocked and ready for battle. Without enough sleep, you’re sending your body into a fight without enough soldiers, leaving you more likely to get sick.”
— Dr. Dylan Petkus.
Heart Health
Poor or insufficient sleep has been linked with high blood pressure, heart failure, arrhythmia, and coronary heart disease. (14, 15, 16, 17) Sleep plays such a vital role in heart health that in 2022, The American Heart Association (AHA) updated its metrics for cardiovascular health. Now a part of Life’s Essential 8™, the AHA says sleep duration (7 to 9 hours of sleep per day for adults) matters for optimal cardiovascular health. (18)
Weight Management
“A lack of sleep can trick your body into feeling hungrier by cranking up the hormone ghrelin (the ‘I’m hungry’ signal) and dialing down leptin (the ‘I’m full’ signal),” says Petkus. Existing research corroborates as much, with newer studies showing that insufficient sleep may derail your weight loss or weight management goals by promoting snacking on high-carbohydrate, high-sugar foods. (19, 20)
Metabolic Health and Insulin Production
While we sleep, our body manages our metabolic health and insulin (the hormone that regulates sugar) production. Petkus explains that when insufficient sleep meddles with our blood sugar control system, the result may be an increased risk for type 2 diabetes. (21) (22)
Hormones, Growth, and Development
“During deep sleep, our bodies release growth hormone, which supports tissue repair, muscle growth, and protein synthesis. (6) Sleep also balances hormones like cortisol — aka, the stress hormone. (8) Petkus says, “Skimp on sleep, and these systems go haywire, making you more stressed and slower to heal.”
Emotional Regulation and Mental Health
Sleep, especially rapid eye movement (REM) sleep, plays a vital role in emotion regulation. (23)
“When you don’t sleep enough, your brain gets glitchy — making you more anxious, moody, and forgetful,” says Petkus, adding, “It’s like trying to run a computer with a bunch of tabs open, and the battery is dying.”
And while sleep plays a heavy hand in managing the psychological effects of stress, research also shows that it plays a key role in mood disorders. One study out of the UK found that healthy sleep decreased the risk of depression by as much as 22 percent, while another found that high-quality sleep can do some pretty heavy lifting to reduce depression and anxiety. (24, 25)
Cognitive Function
Sleep supports cognitive functions like learning, memory consolidation, and brain development. (7, 26, 27) Petkus says we can “Think of sleep as our brain’s overnight cleaning crew. While we’re out for the count, our brain sorts through all the information from our day and makes sense of it.” He goes on to explain that in the absence of quality sleep, our brain may start to feel like a cluttered desk where our focus takes a hit, and it’s impossible to stay organized.
Other cognitive functions supported by sleep include:
Energy Conservation
Researchers are still working to understand sleep fully; in the meantime, we have multiple theories on its purpose.
One theory, called energy conservation theory, suggests that sleep helps our bodies conserve
and restore energy by reducing our metabolic rate (the amount of energy your body uses at a given point in time) at a time when we don’t typically need to call upon our energy stores to get something done. (32,33,34)
Did You Know?
From an evolutionary perspective, The Energy Conservation Theory of sleep suggests that humans slept during the overnight hours to reduce the amount of energy expended during times when it wasn’t efficient or safe to search for food. (33)
Physical Recovery
Another theory on the purpose of sleep suggests that it allows your body to heal courtesy of a growth hormone release that supports muscle growth and tissue repair, cytokines that help with inflammation, and some much-needed downtime. (6,11)
What Happens When We Sleep: Stages Of Sleep
Sleep is divided into two phases: nonrapid eye movement (NREM) sleep and rapid eye movement (REM) sleep. These two phases are then broken down into four stages — N1, N2, N3, and REM. (35) Our bodies repeatedly move through these stages throughout the night in what’s known as a sleep cycle. One sleep cycle lasts about 90 minutes, and people typically go through four to six cycles each night. (35) Day after day, night after night, we move through this sleep-wake cycle, and it’s all regulated by our circadian rhythm, also known as our internal clock. (35)
Stage NREM 1
N1 is the first stage of sleep, where the transition between wakefulness and sleep occurs. (35)
It is the lightest stage of sleep and typically lasts anywhere from one to five minutes. N1 accounts for approximately 5 percent of our total sleep time. (35) During N1 sleep, our muscles begin to relax, and sleepers may be easily awakened. (35)
Stage NREM 2
The second stage of sleep, N2, moves into deeper sleep. N2 accounts for 45 percent of our total sleep time, and its duration changes as the night wears on. While the first N2 stage may last somewhere around 25 minutes, subsequent N2 stages are longer. (35) During N2 sleep, our heart rate and body temperature decrease, our blood pressure drops, and breathing becomes smoother and less erratic. (36)
Stage NREM 3
Also known as slow-wave sleep (SWS), deep sleep, and delta sleep, N3 is the deepest stage of sleep. N3 sleep only accounts for 25 percent of our total sleep time, but it plays a key role in how restored and refreshed we feel upon waking. (35) Moreover, N3 sleep is where critical biological processes like growth hormone release, bone and muscle building, and immune strengthening occur. (35)
REM Sleep
The rapid eye movement stage, or REM sleep, is the fourth and final stage in a sleep cycle. For adults, REM sleep accounts for 25 percent of their total sleep time, and most people will hit their first REM stage somewhere around 60 to 90 minutes into their sleep cycle. (35) Erratic breathing and heart rate, muscle paralysis (muscle atonia), and rapid eye movements (eyes closed, darting back and forth) are hallmark physiological characteristics of REM sleep. (32)
REM sleep is typically considered less restful than other sleep stages, and its duration varies throughout the night. (37) Initial REM stages may be as short as 10 minutes, while the last REM stage of the night could last as long as one hour. (35)
REM sleep is often (and only) linked with dreaming, but there’s plenty more going on during REM sleep. Research shows that REM sleep is responsible for emotion regulation, memory consolidation, and brain development. (23, 26, 27)
How Much Sleep Do I Need?
Hard and fast rules for how much sleep you need are hard to apply because people are so different, age matters, and overall health must be taken into consideration. That said, The American Academy of Sleep Medicine (AASM) outlines the following sleep recommendations by age range. (1)
| Age Group | Age Range | Recommended Hours of Sleep |
| Infant | 4 – 12 months | 12 – 16 hours (including naps) |
| Toddler | 1 – 2 years | 11 – 14 hours (including naps) |
| Preschool | 3 – 5 years | 10 – 13 hours (including naps) |
| School Age | 6 – 12 years | 9 – 12 hours |
| Teen | 13 – 18 years | 8 – 10 hours |
| Adult | 18+ years | 7 or more hours |
Note: The American Academy of Sleep Medicine (AASM) doesn’t provide specific sleep recommendations for newborns under four months old because of limited data and the wide range of normal sleep patterns for this age group.
What If I Don’t Get Enough Sleep?
Across a lifetime, we’re all subject to a sleepless night from time to time, which is usually no cause for concern. Prolonged bouts of sleep deprivation, however, can lead to a series of health concerns and chronic issues if left untreated. In summation, Petkus tells us, “A lack of sleep can lead to poor decision-making, a weakened immune system, and even long-term health problems like heart disease and diabetes.”
Short-term sleep deprivation may cause: (38)
- Excessive daytime sleepiness/fatigue (39)
- Moodiness/Irritability (39)
- Delayed reaction times (39)
- Poor focus/concentration (39)
- Impaired memory (40)
Long-term sleep deprivation may include increased risk of: (38)
- Depression (41)
- Anxiety (41)
- Impaired cognitive function (42)
- Type 2 diabetes (43)
- Obesity (44)
- Stroke (45)
- Cardiovascular disease (46)
- Heart attack (46)
Getting Better Sleep: What to Know About Sleep Hygiene
For those struggling with healthy sleep, improved sleep hygiene (behaviors and habits that promote a good night’s sleep) practices may be the key to getting a good night’s sleep.
If you’re a little late to the slumber party, here are some tips for better sleep.
Maintain a Consistent Sleep Schedule
Maintaining a consistent sleep schedule is a key component of healthy sleep. This means going to bed and waking up at the same time every day (even on weekends) and ensuring that your sleep schedule allows for seven to nine hours of sleep per night.
Create a Relaxing Bedtime Routine
Swapping your nightly doomscroll for calming activities before bedtime can help you relax. With consistency over time, bedtime routines will eventually signal your body that it’s time for sleep. (47)
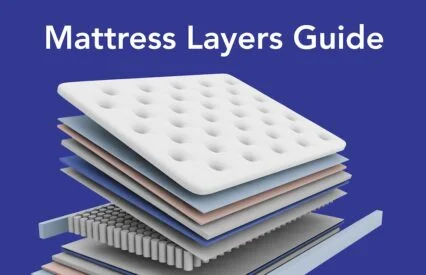
Optimize Your Sleep Space
One of the key principles of sleep hygiene is ensuring your sleep space is cool, dark, and quiet. (48) Sleep masks and blackout curtains may prove helpful for managing light, and colored noise may help drown out ambient noise. Optimizing your sleep space may also include reassessing your mattress, pillows, and sheets and tailoring them to your needs.
Watch What You Eat and Drink Before Bed
Sleep experts agree that eating heavy meals and consuming caffeine and alcohol before bed is a no-no. Studies show that caffeine can make it harder to fall asleep and reduce overall sleep time. (49) Similarly, ill-timed meals can impair sleep quality and duration, and while alcohol may help you fall asleep faster, frequent waking and restlessness are likely as your nightcap continues to impact your body throughout the night. (48, 50)
Limit Screen Time
Blue light exposure from smartphones, TVs, and other devices can disrupt the production of melatonin (the sleep hormone) and compromise your sleep quality. (51) To mitigate these risks, consider limiting your screen time in the evening and completely disconnecting one hour before lights out. (51)
Get Regular Exercise
Regular exercise can help alleviate stress and anxiety and improve sleep. Just don’t do anything too rigorous close to bedtime — yoga, for instance, may be a better close-to-bedtime activity than kickboxing. (52, 53, 54)
FAQs
What is the purpose of sleep?
Physically, sleep plays a key role in our body’s growth and repair processes. Emotionally and mentally, sleep regulates our emotions and keeps our cognitive function sharp.
Why is sleep important?
Sleep is important because our bodies carry out a host of biological and physiological processes during the overnight hours. While good quality sleep leaves us feeling refreshed and restored upon waking, it also supports healthy immune function, heart health, weight management, brain function, and mental health.
What happens if we don’t sleep?
A sleepless night here and there is usually no cause for concern, but prolonged bouts of sleep deprivation can lead to a host of acute health concerns and chronic issues if left untreated. The effects of sleep deprivation over the short term may include headaches, fatigue, irritability, and poor focus. Long-term effects of sleep deprivation may include heart disease, diabetes, obesity, and blunted cognitive function.
The Last Word From Sleepopolis
If there’s anything to learn from the science of sleep, it’s that sleep is anything but unnecessary. While we’re out for the count each night, our bodies are busy getting our house in order for whatever life throws our way. Just remember, sleep and health go hand in hand — take care of one, and you’ll take care of the other.
Sources
- Sleep faqs. Sleep Education. (2021, May 4). https://sleepeducation.org/sleep-faqs/
- Foy, S. F. and D. (2024b, April 26). Americans sleeping less, more stressed. Gallup.com. https://news.gallup.com/poll/642704/americans-sleeping-less-stressed.aspx
- Khubchandani, J., Price, J.H. Short Sleep Duration in Working American Adults, 2010–2018. J Community Health 45, 219–227 (2020). https://doi.org/10.1007/s10900-019-00731-9
- U.S. Department of Health and Human Services. (n.d.). Brain basics: Understanding sleep. National Institute of Neurological Disorders and Stroke. https://www.ninds.nih.gov/health-information/public-education/brain-basics/brain-basics-understanding-sleep
- Science of sleep: What is sleep? Sleep Medicine. (n.d.). https://sleep.hms.harvard.edu/education-training/public-education/sleep-and-health-education-program/sleep-health-education-47
- Zaffanello, M., Pietrobelli, A., Cavarzere, P., Guzzo, A., & Antoniazzi, F. (2024). Complex relationship between growth hormone and sleep in children: Insights, discrepancies, and implications. Frontiers in Endocrinology, 14, 1332114. https://doi.org/10.3389/fendo.2023.1332114
- Lendner, J. D., Niethard, N., Mander, B. A., Schuh-Hofer, S., Schmidt, H., Knight, R. T., Born, J., Walker, M. P., Lin, J. J., & Helfrich, R. F. (2023). Human REM sleep recalibrates neural activity in support of memory formation. Science Advances. https://doi.org/adj1895
- Yap, Y., Tung, N. Y., Shen, L., Bei, B., Phillips, A., & Wiley, J. F. (2024). Daily associations between salivary cortisol and electroencephalographic-assessed sleep: A 15-day intensive longitudinal study. Sleep, 47(9). https://doi.org/10.1093/sleep/zsae087
- U.S. Department of Health and Human Services. (n.d.). How sleep affects your health. National Heart Lung and Blood Institute. https://www.nhlbi.nih.gov/health/sleep-deprivation/health-effects
- Gilley, R. R. (2022). The Role of Sleep in Cognitive Function: The Value of a Good Night’s Rest. Clinical EEG and Neuroscience. https://doi.org/10.1177/15500594221090067
- NCI Dictionary of Cancer terms. Comprehensive Cancer Information – NCI. (n.d.). https://www.cancer.gov/publications/dictionaries/cancer-terms/def/cytokine
- Garbarino S, Lanteri P, Bragazzi NL, Magnavita N, Scoditti E. Role of sleep deprivation in immune-related disease risk and outcomes. Commun Biol. 2021;4(1):1304. Published 2021 Nov 18. doi:10.1038/s42003-021-02825-4
- Martínez-Albert, E., Lutz, N. D., Hübener, R., Dimitrov, S., Lange, T., Born, J., & Besedovsky, L. (2024). Sleep promotes T-cell migration towards CCL19 via growth hormone and prolactin signaling in humans. Brain, Behavior, and Immunity, 118, 69-77. https://doi.org/10.1016/j.bbi.2024.02.021
- Centers for Disease Control and Prevention. (n.d.). About sleep and your heart health. Centers for Disease Control and Prevention. https://www.cdc.gov/heart-disease/about/sleep-and-heart-health.html
- Zheng, T. (2021). Sleep disturbance in heart failure: A concept analysis. Nursing Forum, 56(3), 710. https://doi.org/10.1111/nuf.12566
- Gaffey, A. E., Rosman, L., Lampert, R., Yaggi, H. K., Haskell, S. G., Brandt, C. A., Enriquez, A. D., Mazzella, A. J., Skanderson, M., & Burg, M. M. (2023). Insomnia and early incident atrial fibrillation: A 16‐year cohort study of younger men and women veterans. Journal of the American Heart Association, 12(20). https://doi.org/10.1161/jaha.123.030331
- Wei, R., Duan, X., & Guo, L. (2022). Effects of sleep deprivation on coronary heart disease. The Korean Journal of Physiology & Pharmacology: Official Journal of the Korean Physiological Society and the Korean Society of Pharmacology, 26(5), 297-305. https://doi.org/10.4196/kjpp.2022.26.5.297
- Life’s essential 8. www.heart.org. (n.d.). https://www.heart.org/en/healthy-living/healthy-lifestyle/lifes-essential-8
- Zhu B, Shi C, Park CG, Zhao X, Reutrakul S. Effects of sleep restriction on metabolism-related parameters in healthy adults: A comprehensive review and meta-analysis of randomized controlled trials. Sleep Med Rev. 2019 Jun;45:18-30. doi: 10.1016/j.smrv.2019.02.002. Epub 2019 Feb 10. PMID: 30870662.
- Potosky, E., Taylor, C., Wexler, R., & Pratt, K. (2021). Differences in Snacking Intakes by Meeting Sleep Recommendations. Journal of the Academy of Nutrition and Dietetics, 121(9), A52. https://doi.org/10.1016/j.jand.2021.06.145
- Fabia M. Stich, Stephanie Huwiler, Gommaar D’Hulst, Caroline Lustenberger; The Potential Role of Sleep in Promoting a Healthy Body Composition: Underlying Mechanisms Determining Muscle, Fat, and Bone Mass and Their Association with Sleep. Neuroendocrinology 1 July 2022; 112 (7): 673–701. https://doi.org/10.1159/000518691
- Nôga DA, Meth EDMES, Pacheco AP, et al. Habitual Short Sleep Duration, Diet, and Development of Type 2 Diabetes in Adults. JAMA Netw Open. 2024;7(3):e241147. doi:10.1001/jamanetworkopen.2024.1147
- Galbiati, A., Sforza, M., Fasiello, E., Casoni, F., Marrella, N., Leitner, C., Zucconi, M., & Ferini-Strambi, L. (2020). The association between emotional dysregulation and REM sleep features in insomnia disorder. Brain and Cognition, 146, 105642. https://doi.org/10.1016/j.bandc.2020.105642
- Li Y, Sahakian BJ, Kang J, et al. The brain structure and genetic mechanisms underlying the nonlinear association between sleep duration, cognition and mental health [published correction appears in Nat Aging. 2022 May;2(5):453. doi: 10.1038/s43587-022-00230-y]. Nat Aging. 2022;2(5):425-437. doi:10.1038/s43587-022-00210-2
- Sullivan, E. C., James, E., Henderson, L., McCall, C., & Cairney, S. A. (2023). The influence of emotion regulation strategies and sleep quality on depression and anxiety. Cortex, 166, 286-305. https://doi.org/10.1016/j.cortex.2023.06.001
- Simon, K. C., Nadel, L., & Payne, J. D. (2022). The functions of sleep: A cognitive neuroscience perspective. Proceedings of the National Academy of Sciences, 119(44). https://doi.org/10.1073/pnas.2201795119
- Fan Jiang; Sleep and Early Brain Development. Ann Nutr Metab 28 December 2019; 75 (Suppl. 1): 44–54. https://doi.org/10.1159/000508055
- Dutheil, F., Danini, B., Bagheri, R., Fantini, M. L., Pereira, B., Moustafa, F., Trousselard, M., & Navel, V. (2021). Effects of a Short Daytime Nap on the Cognitive Performance: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 18(19). https://doi.org/10.3390/ijerph181910212
- Brunet, J., McNeil, J., Doucet, É., & Forest, G. (2020). The association between REM sleep and decision-making: Supporting evidences. Physiology & Behavior, 225, 113109. https://doi.org/10.1016/j.physbeh.2020.113109
- Calechman, S. (2021, May 24). Sleep to solve a problem. Harvard Health. https://www.health.harvard.edu/blog/sleep-to-solve-a-problem-202105242463
- Lacaux, C., Andrillon, T., Bastoul, C., Idir, Y., Fonteix-Galet, A., Arnulf, I., & Oudiette, D. (2021). Sleep onset is a creative sweet spot. Science Advances. https://doi.org/abj5866
- Metabolic rate. Oxford Reference. (n.d.). https://www.oxfordreference.com/display/10.1093/oi/authority.20110810105405374
- Brinkman JE, Reddy V, Sharma S. Physiology of Sleep. [Updated 2023 Apr 3]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482512/
- Lesku, J. A., & Schmidt, M. H. (2022). Energetic costs and benefits of sleep. Current Biology, 32(12), R656-R661. https://doi.org/10.1016/j.cub.2022.04.004
- Patel AK, Reddy V, Shumway KR, et al. Physiology, Sleep Stages. [Updated 2024 Jan 26]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK526132/
- Helakari, H., Järvelä, M., Väyrynen, T., Tuunanen, J., Piispala, J., Kallio, M., Ebrahimi, S. M., Poltojainen, V., Kananen, J., Elabasy, A., Huotari, N., Raitamaa, L., Tuovinen, T., Korhonen, V., Nedergaard, M., & Kiviniemi, V. (2023). Effect of sleep deprivation and NREM sleep stage on physiological brain pulsations. Frontiers in Neuroscience, 17, 1275184. https://doi.org/10.3389/fnins.2023.1275184
- Martin, J. M., Andriano, D. W., Mota, N. B., Mota-Rolim, S. A., Araújo, J. F., Solms, M., & Ribeiro, S. (2020). Structural differences between REM and non-REM dream reports assessed by graph analysis. PLOS ONE, 15(7), e0228903. https://doi.org/10.1371/journal.pone.0228903
- U.S. Department of Health and Human Services. (n.d.-b). What are sleep deprivation and deficiency? National Heart Lung and Blood Institute. https://www.nhlbi.nih.gov/health/sleep-deprivation
- Thompson, K. I., Chau, M., Lorenzetti, M. S., Hill, L. D., Fins, A. I., & Tartar, J. L. (2022). Acute sleep deprivation disrupts emotion, cognition, inflammation, and cortisol in young healthy adults. Frontiers in Behavioral Neuroscience, 16, 945661. https://doi.org/10.3389/fnbeh.2022.945661
- Newbury, C. R., Crowley, R., Rastle, K., & Tamminen, J. (2021). Sleep deprivation and memory: Meta-analytic reviews of studies on sleep deprivation before and after learning. Psychological Bulletin, 147(11), 1215–1240. https://doi.org/10.1037/bul0000348
- Uccella, S., Cordani, R., Salfi, F., Gorgoni, M., Scarpelli, S., Gemignani, A., Geoffroy, P. A., De Gennaro, L., Palagini, L., Ferrara, M., & Nobili, L. (2023). Sleep Deprivation and Insomnia in Adolescence: Implications for Mental Health. Brain Sciences, 13(4), 569. https://doi.org/10.3390/brainsci13040569
- Hudson, A.N., Van Dongen, H.P.A. & Honn, K.A. Sleep deprivation, vigilant attention, and brain function: a review. Neuropsychopharmacol. 45, 21–30 (2020). https://doi.org/10.1038/s41386-019-0432-6
- Nôga DA, Meth EDMES, Pacheco AP, et al. Habitual Short Sleep Duration, Diet, and Development of Type 2 Diabetes in Adults. JAMA Netw Open. 2024;7(3):e241147. doi:10.1001/jamanetworkopen.2024.1147
- Akhlaghi M, Kohanmoo A. Sleep deprivation in development of obesity, effects on appetite regulation, energy metabolism, and dietary choices. Nutrition Research Reviews. Published online 2023:1-21. doi:10.1017/S0954422423000264
- Koo DL, Nam H, Thomas RJ, Yun CH. Sleep Disturbances as a Risk Factor for Stroke. J Stroke. 2018;20(1):12-32. doi:10.5853/jos.2017.02887
- Wei R, Duan X, Guo L. Effects of sleep deprivation on coronary heart disease. Korean J Physiol Pharmacol. 2022;26(5):297-305. doi:10.4196/kjpp.2022.26.5.297
- Foster RG. Sleep, circadian rhythms and health. Interface Focus. 2020;10(3):20190098. doi:10.1098/rsfs.2019.0098
- Iao SI, Jansen E, Shedden K, et al. Associations between bedtime eating or drinking, sleep duration and wake after sleep onset: findings from the American time use survey. Br J Nutr. Published online September 13, 2021. doi:10.1017/S0007114521003597
- Gardiner C, Weakley J, Burke LM, Roach GD, Sargent C, Maniar N, Townshend A, Halson SL. The effect of caffeine on subsequent sleep: A systematic review and meta-analysis. Sleep Med Rev. 2023 Jun;69:101764. doi: 10.1016/j.smrv.2023.101764. Epub 2023 Feb 6. PMID: 36870101.
- Jones, M. R., Brandner, A. J., Vendruscolo, L. F., Vendruscolo, J. C., Koob, G. F., & Schmeichel, B. E. (2022). Effects of Alcohol Withdrawal on Sleep Macroarchitecture and Microarchitecture in Female and Male Rats. Frontiers in Neuroscience, 16, 838486. https://doi.org/10.3389/fnins.2022.838486
- Siraji MA, Spitschan M, Kalavally V, Haque S. Light exposure behaviors predict mood, memory and sleep quality. Sci Rep. 2023;13(1):12425. Published 2023 Aug 1. doi:10.1038/s41598-023-39636-y
- Lin, Y., & Gao, W. (2023). The effects of physical exercise on anxiety symptoms of college students: A meta-analysis. Frontiers in Psychology, 14, 1136900. https://doi.org/10.3389/fpsyg.2023.1136900
- Zapalac K, Miller M, Champagne FA, Schnyer DM, Baird B. The effects of physical activity on sleep architecture and mood in naturalistic environments. Sci Rep. 2024;14(1):5637. Published 2024 Mar 7. doi:10.1038/s41598-024-56332-7
- Stutz J, Eiholzer R, Spengler CM. Effects of Evening Exercise on Sleep in Healthy Participants: A Systematic Review and Meta-Analysis. Sports Med. 2019 Feb;49(2):269-287. doi: 10.1007/s40279-018-1015-0. PMID: 30374942.
Petkus, Dylan. Author Interview. September 16, 2024.